Updates in Pustular Psoriasis
Megan H. Noe, MD, MPH, MSCE
Assistant Professor of Dermatology, Brigham and Women’s Hospital (founder), Harvard Medical School
August 2023
Dr. Noe presented an overview of pustular psoriasis and treatment options.
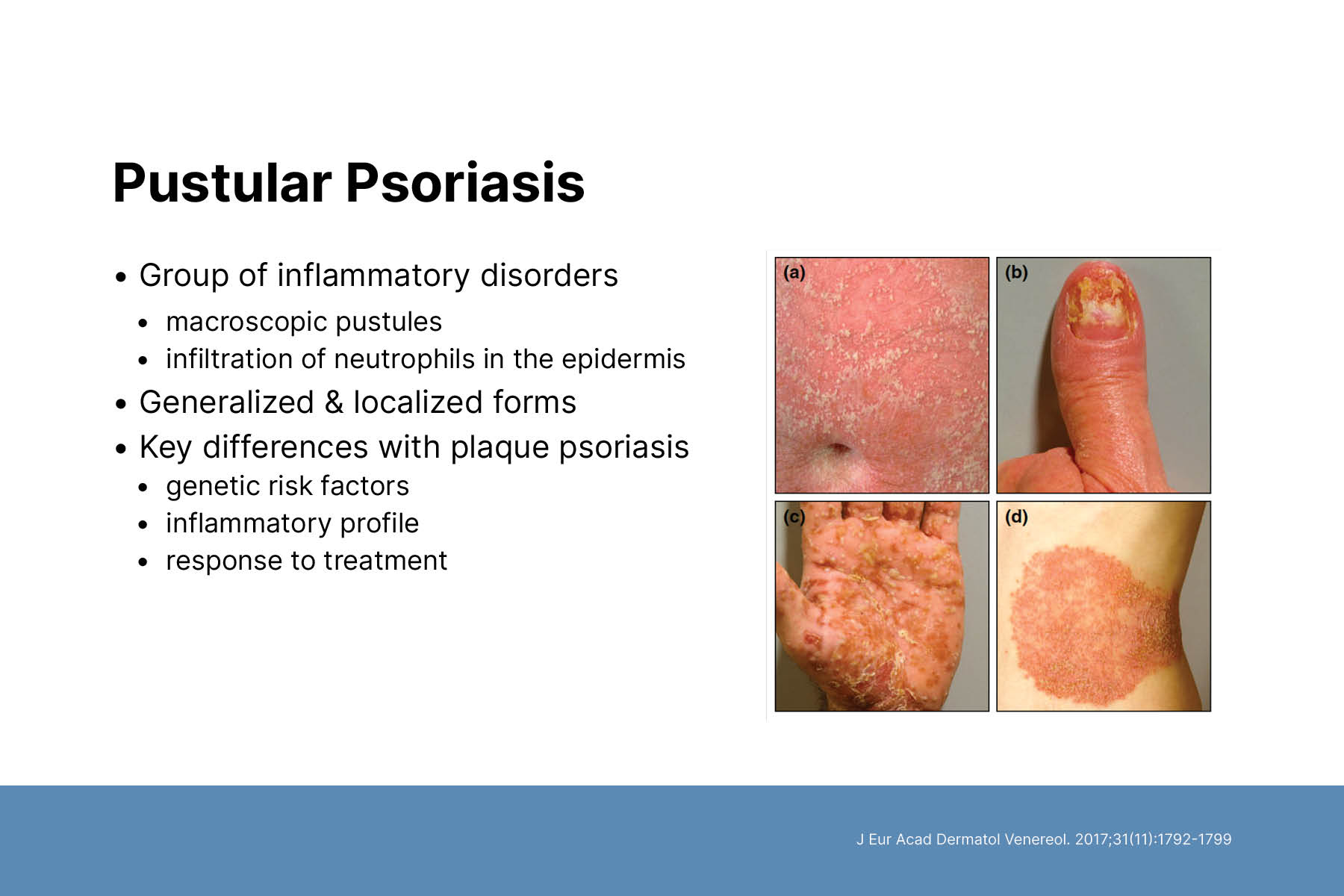
Pustular psoriasis is a group of inflammatory skin diseases characterized by visible, sterile pustules on inflamed skin. It appears in generalized and localized forms and can occur in patients with or without a history of psoriasis. Pustular psoriasis has distinct genetic risk factors, inflammatory profile, and response to treatment compared to psoriasis. Thus, it may be its own unique disease.
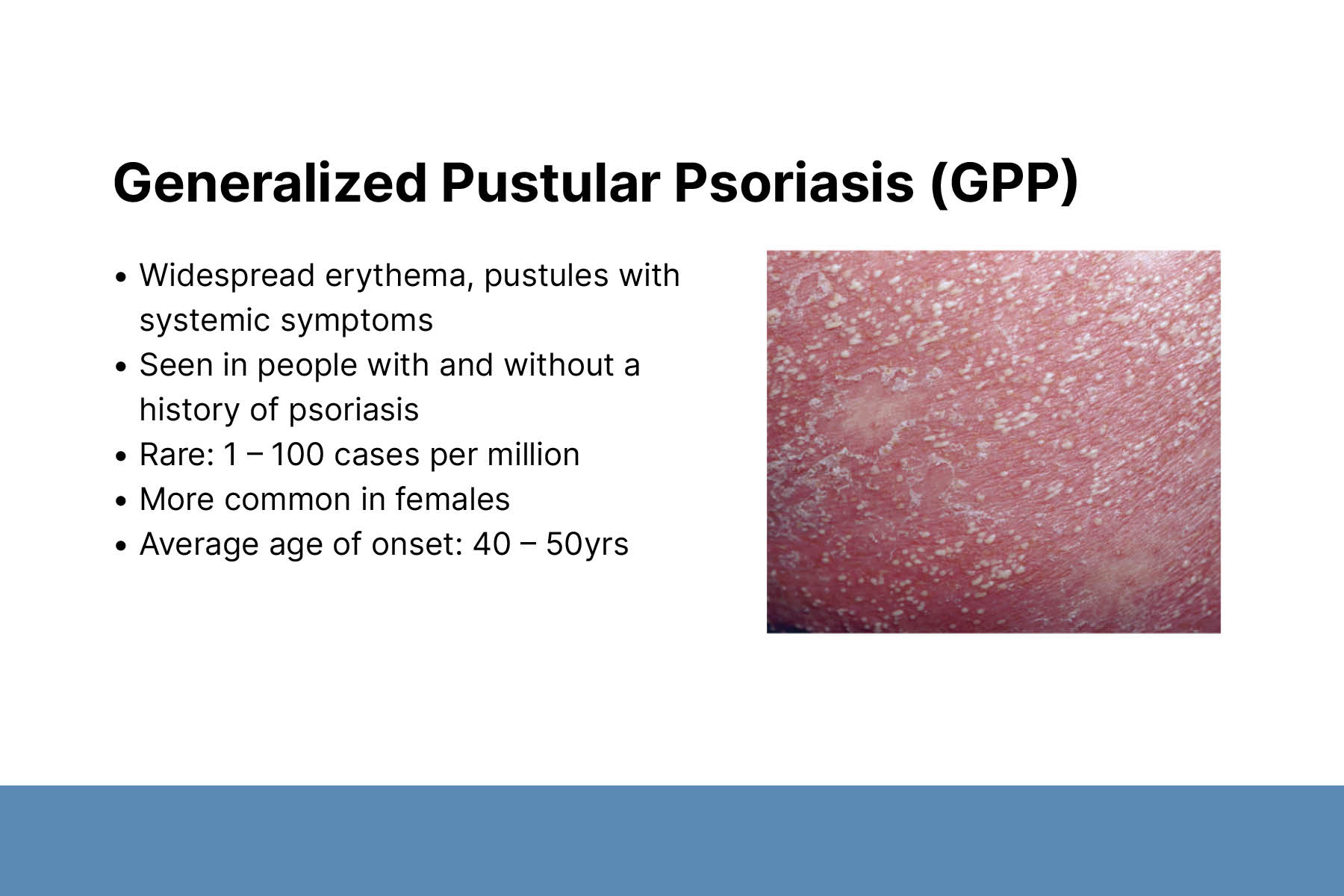
Generalized pustular psoriasis (GPP) is characterized by the rapid appearance of sterile pustules and generalized erythema (skin reddening). It is a diverse disease, which varies widely in severity and clinical course. Recognizing the distinctive and broad range of GPP manifestations enables prompt diagnosis and timely treatment.
Genetic mutations have been identified in some GPP cases, including IL36RN, CARD14, AP1S3, SERPINA3 and MPO. Interleukin 36 (IL-36) signaling has been identified as a key pathway driving GPP. Early-onset GPP without preceding plaque psoriasis is often associated with IL36RN mutations.
High-quality evidence to guide treatment decisions for GPP is lacking. Limited efficacy and safety evidence is available for widely used treatments such as acitretin, methotrexate, cyclosporin, and biologics. Biologics indicated for psoriasis, including guselkumab and adalimumab have limited efficacy in GPP. Dr. Noe described ongoing clinical trials of the IL-36 receptor antagonists spesolimab and imsidolimab.
Pregnancy-associated GPP is clinically indistinguishable from other types of GPP. It typically presents in the third trimester and resolves after delivery. There is an increased risk of earlier, more severe outbreaks in subsequent pregnancies. Pregnancy-associated GPP is associated with miscarriage, fetal growth restriction, and premature labor. Immediate treatment and fetal monitoring are recommended. Treatment options include corticosteroids, cyclosporin, and infliximab.
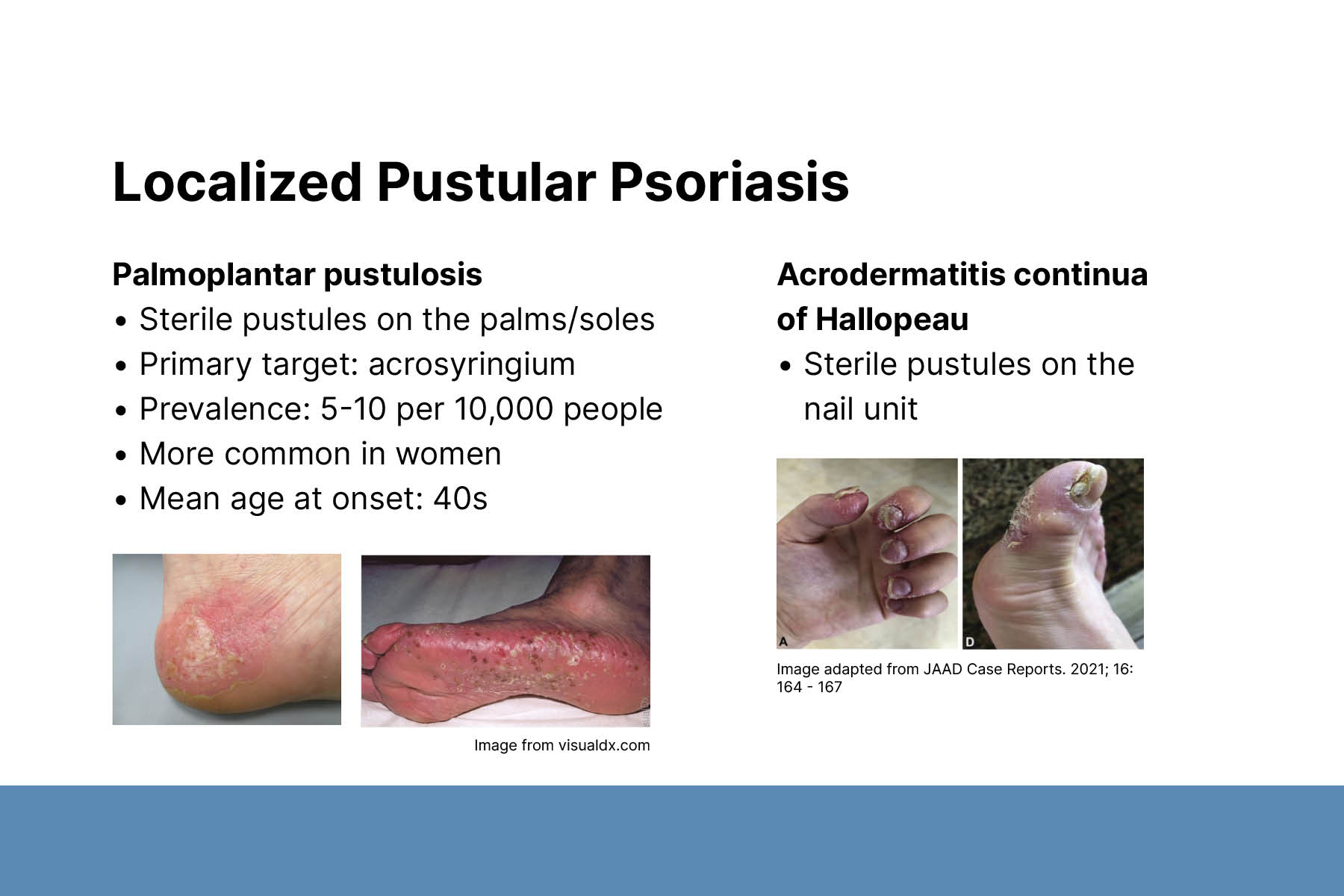
Localized pustular psoriasis includes acrodermatitis continua of Hallopeau (ACH) and palmoplantar pustulosis (PPP). ACH is a chronic, relapsing, inflammatory nail disease. It can be seen alone or with other forms of pustular psoriasis. IL36RN mutations have been identified in ACH. Little is known about ACH as a solitary disease.
PPP is characterized by sterile pustules on the palms and soles. There is no consensus on optimal treatment for PPP. Common treatments include acitretin, methotrexate, and phototherapy. Identified mutations in PPP share some overlap with GPP, with lower frequency of IL36RN mutations. PPP is not associated with the psoriasis risk allele PSORS1. There is some evidence for a genetic link between PPP and psoriasis.