The Melanoma Epidemic: Real or Illusory
Adewole S. Adamson, MD, MPP
Assistant Professor, Division of Dermatology, Department of Internal Medicine,
Dell Medical School, University of Texas at Austin
August 2023
Dr. Adamson presented information about the risks and benefits of melanoma screening and overdiagnosis.
First, Dr. Adamson addressed the hypothesis that the rising incidence of melanoma is caused by increased UV exposure. Since 1975, the incidence of melanoma has increased by 400% in white women and 600% in white men. While Dr. Adamson agrees there is an association between sun exposure and melanoma, sun exposure cannot explain most of the increase in incidence.
An Australian public health program to promote sun protective behaviors showed an increase in these behaviors and a decrease in non-melanoma skin cancer rates. However, there was no significant change in melanoma incidence trends. There is evidence that sunburn history doubles the risk of melanoma; sunscreen can reduce that risk albeit moderately in absolute terms.
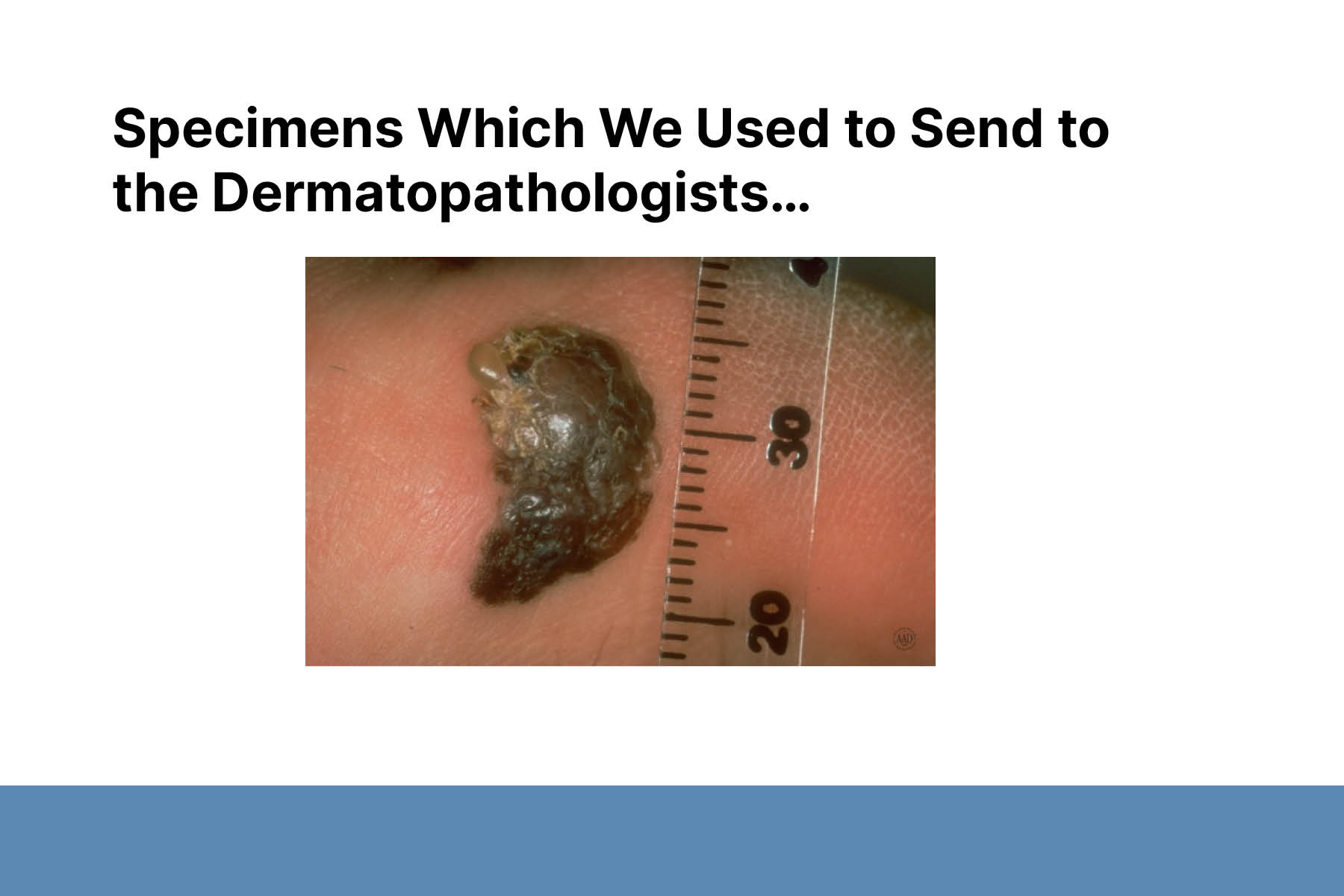
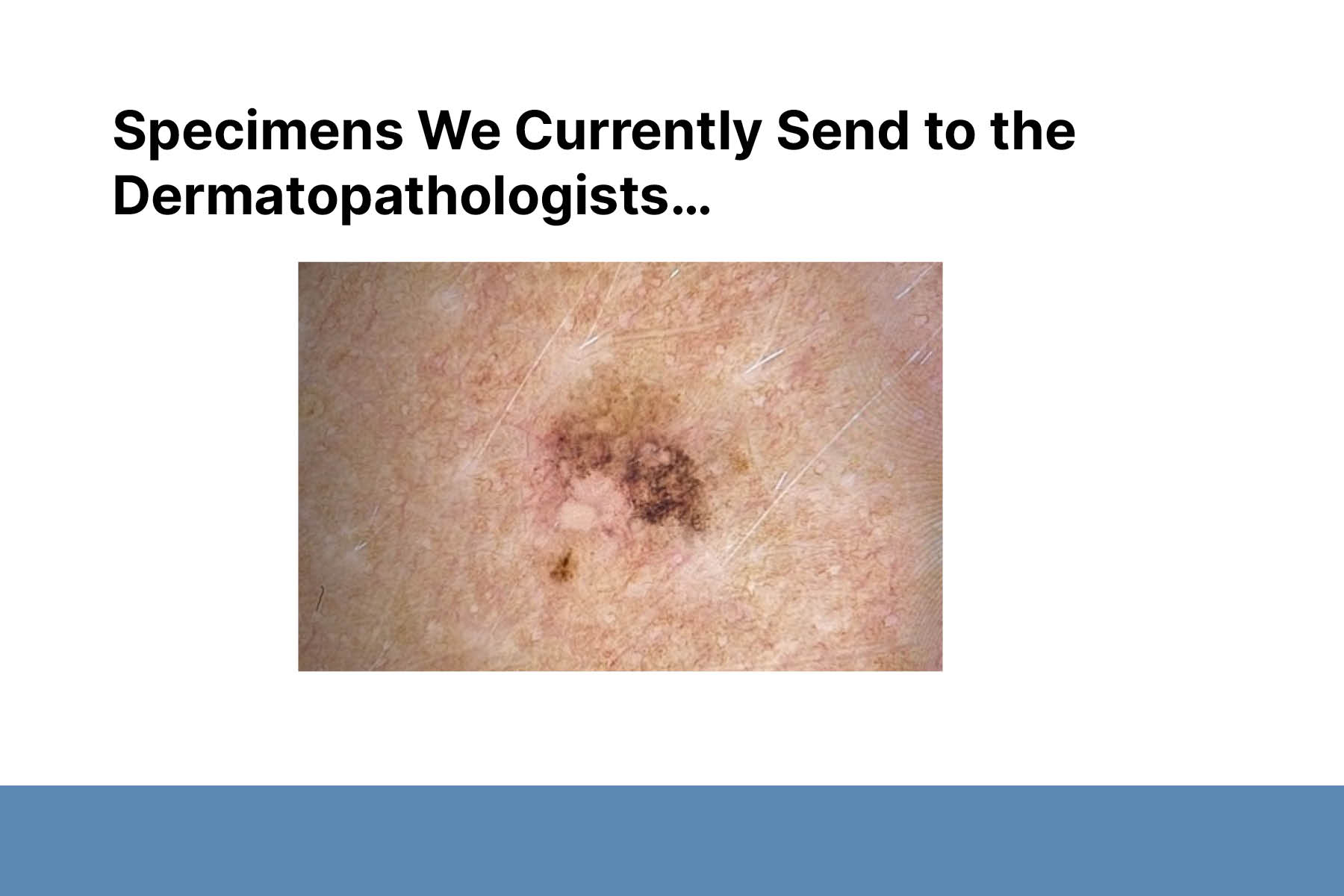
Second, Dr. Adamson proposed overdiagnosis as an alternative explanation for much of the increased incidence of melanoma. Overdiagnosis is defined as the diagnosis of disease that will never cause symptoms or death during a patient’s ordinarily expected lifetime. Despite the increase in melanoma incidence in the past 40 years, melanoma-related mortality rates have remained roughly the same. These are epidemiologic features concerning for overdiagnosis.
Third, Dr. Adamson discussed the possible benefits and harms of melanoma screening. Possible benefits include reducing mortality and recurrence rates and increasing risk reduction behaviors. Potential harms include false positives leading to unnecessary treatment, false negatives leading to faulty reassurance, and increased worry for patients and those around them. Strong evidence for the benefits of screening is needed before exposing many healthy people to its possible harms. Currently, the benefits of melanoma screening and the harmful effects of screening (including overdiagnosis) are poorly understood.
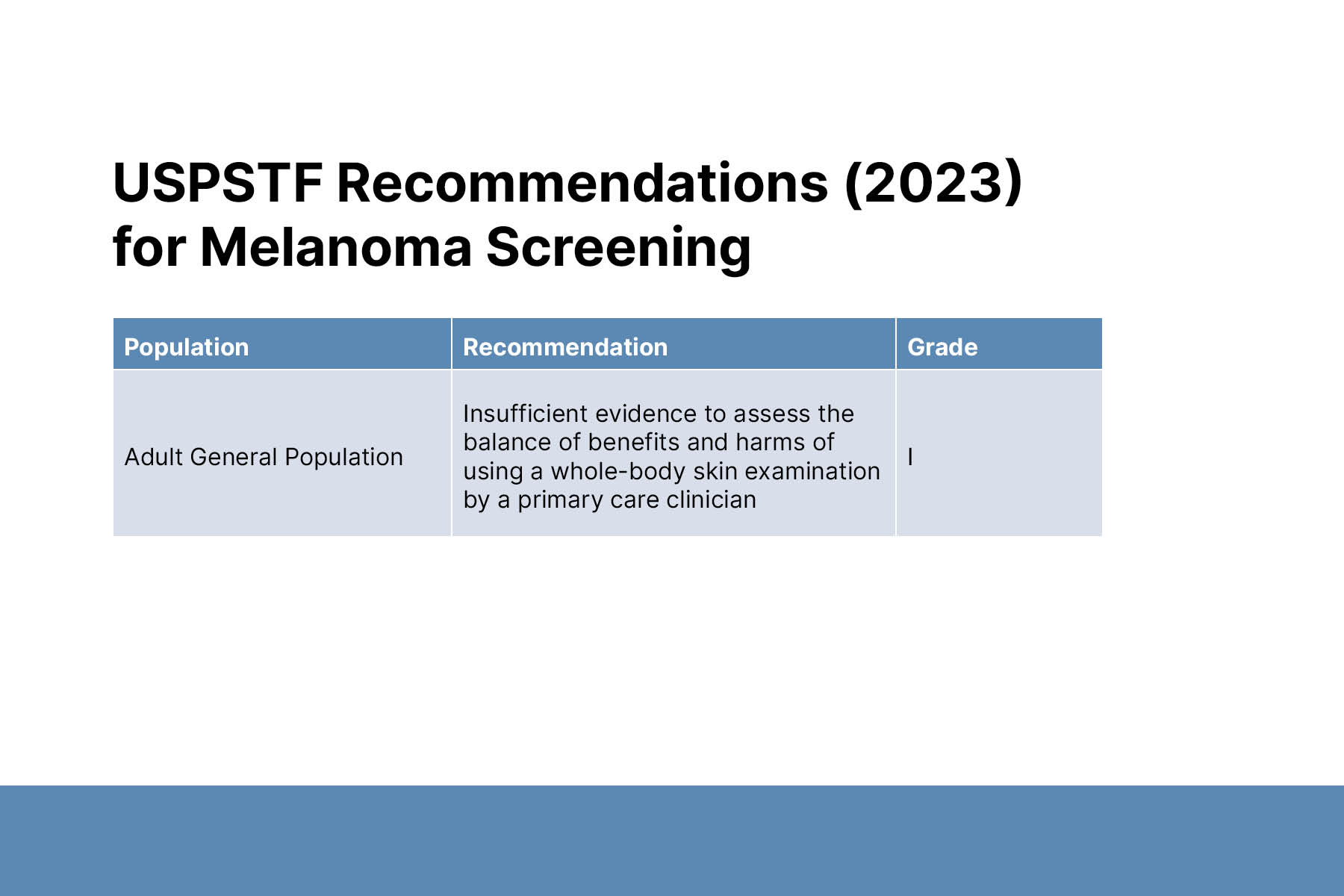
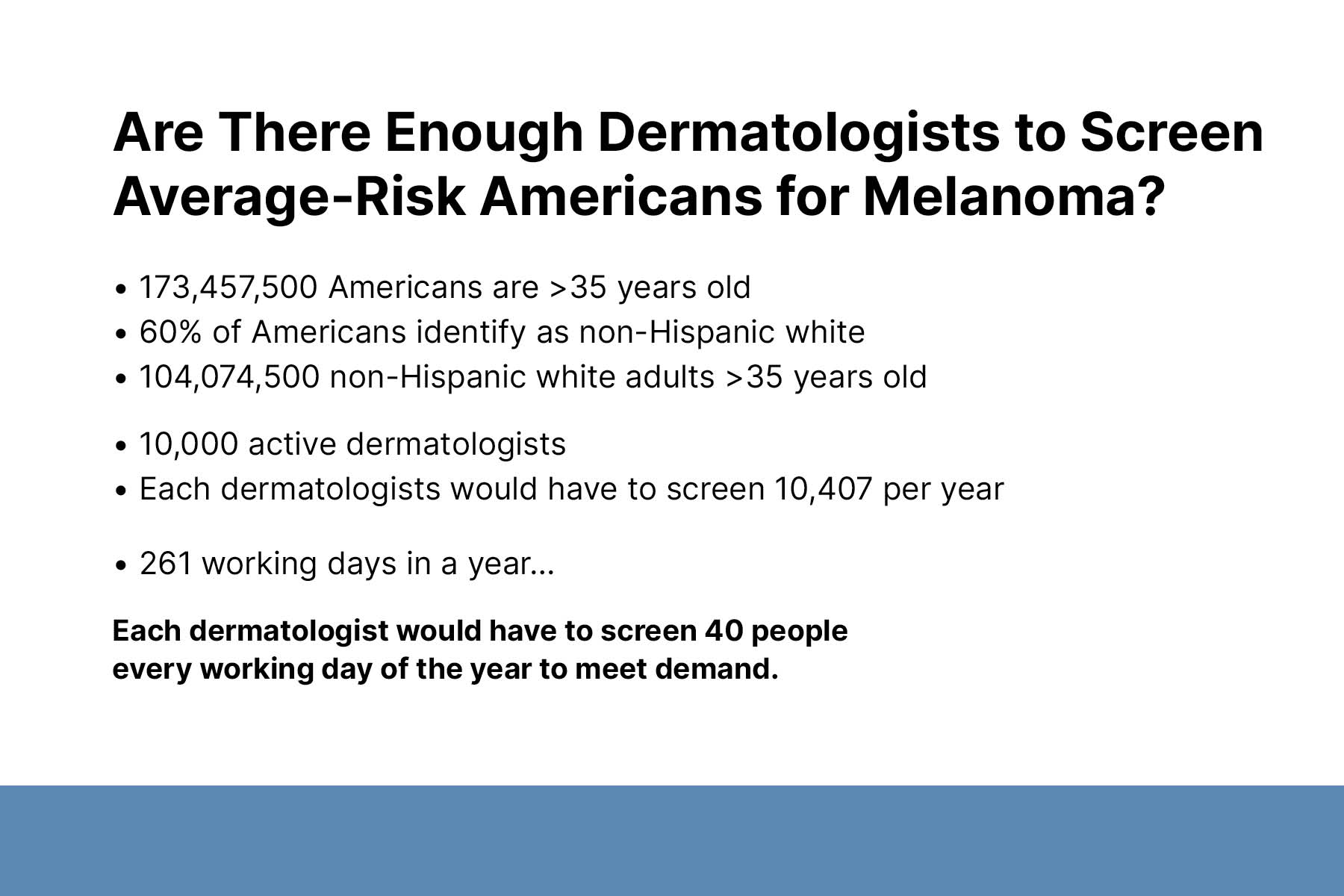
In 2023, the United States Preventive Services Task Force determined there was insufficient evidence to assess the balance of benefits and harms of screening for melanoma using a whole-body skin examination in the primary care setting in part due to the lack of randomized controlled studies. Such studies addressing the mortality benefit of screening for skin cancer would be a massive undertaking. On a practical level, there are not enough dermatologists in the country to screen all American adults for skin cancer.
To conclude, Dr. Adamson reiterated that overdiagnosis of melanoma is a problem. There is limited evidence for the effectiveness of melanoma screening in the general population. The benefits of targeted screening for people with significant risk factors warrant further research.