Skin Cancer Disparities in Patients with Skin of Color
Adewole S. Adamson, MD, MPP
Assistant Professor, Division of Dermatology, Department of Internal Medicine, Dell Medical School, University of Texas at Austin
August 2023
Dr. Adamson presented about skin cancer disparities in patients with skin of color.
First, Dr. Adamson described the epidemiology of skin cancers in patients with skin of color. The incidence of basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma is significantly lower in darker skin types. In Black people, BCC is 2000-fold less common, and SCC is 500-1000-fold less common compared to non-Hispanic white people. Melanoma-related mortality rates in the US-based Black population has been declining during the past 20 years. Non-white race is associated with later melanoma detection and lower survival rates. Multiple risk factors have been proposed for skin cancers in skin of color including immunosuppression and previous scarring. More research is needed to understand the primary drivers of skin cancer in skin of color.
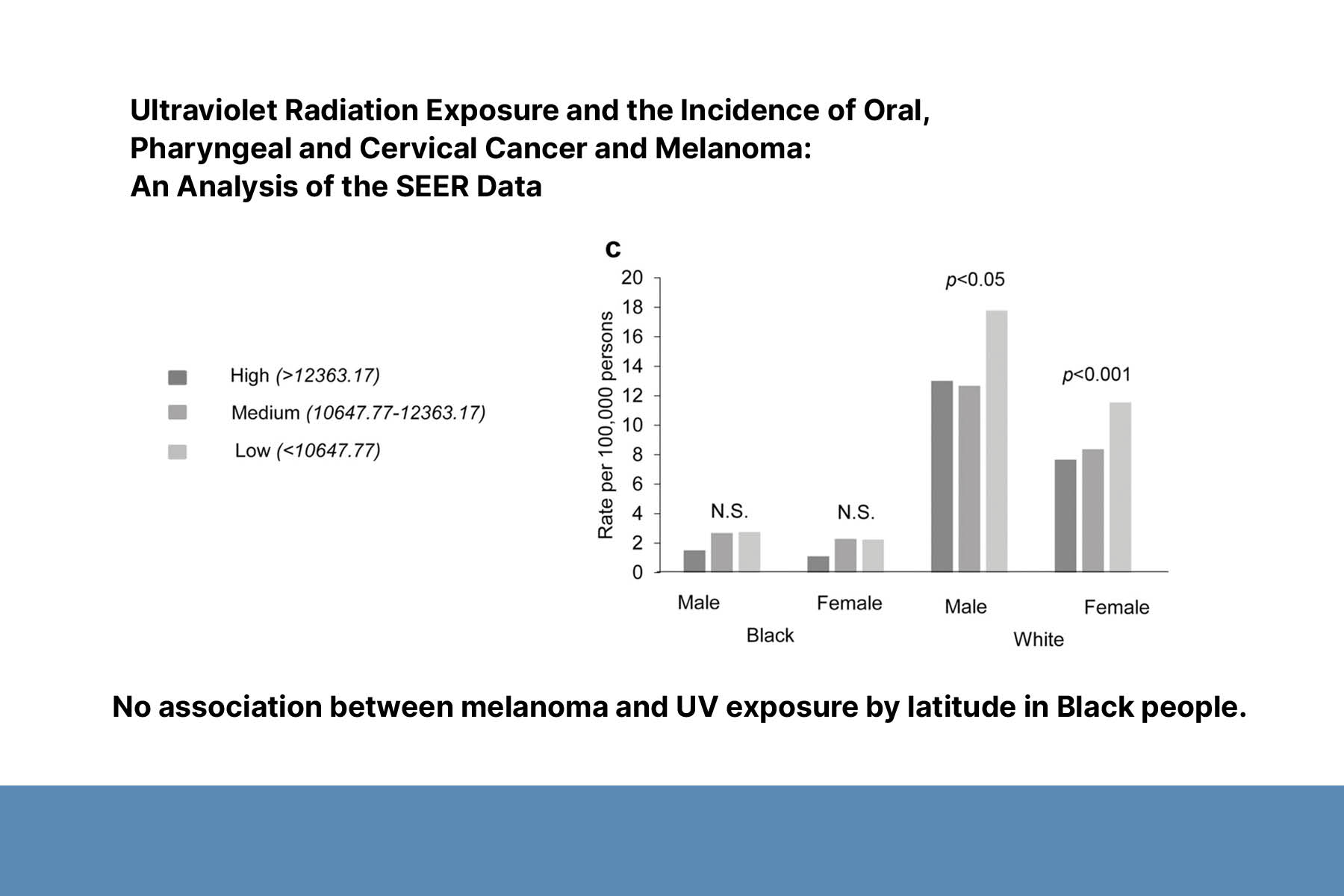
Second, Dr. Adamson discussed the association between UV exposure and skin cancer in skin of color. UV exposure is the primary modifiable risk factor associated with skin cancer in white populations. Dr. Adamson conducted two systematic reviews and found limited evidence that UV exposure is a causal factor in the development of skin cancers in patients with skin of color. There is no evidence that photoprotection reduces melanoma risk in skin of color.
Third, Dr. Adamson shared his research on melanoma treatment disparities. This research analyzed the North Carolina Cancer Information and Population Health Resource database linking patient and tumor information with claims data. Results showed that surgical delays were common regardless of insurance type (Private/Medicare/Medicaid). Surgical delay was defined as a period of more than 6 weeks from diagnosis to definitive melanoma surgery. Fewer delays were noted in patients who were diagnosed or operated on by a dermatologist. Patients of color were 38% more likely to experience surgical delays. Surgical delays impacted survival of patient with melanoma.
Additional findings showed disparities in the use of systemic therapies and immunotherapies. Patients with Medicaid insurance were 30% and 43% less likely to receive systemic therapy and immunotherapy for metastatic melanoma than those with private insurance. Medicaid patients were 45% less likely to receive immunotherapy for metastatic melanoma compared to Medicare patients. The causes of these disparities remain unknown. In future research, Dr. Adamson hopes to identify patient- and provider-reported factors that contribute to delayed or low-quality care.
To conclude, Dr. Adamson stated that non-UV-based nuanced messaging is needed to increase skin cancer awareness among patients with darker skin types and ensure equitable, timely access to evidence-based care.