Top 10 Tips for Treating Skin Disease in Children with Cancer
Jennifer T. Huang, MD
Section Chief, Dermatology, Boston Children’s Hospital, Associate Professor of Dermatology,
Harvard Medical School
August 2023
Dr. Huang presented 10 tips for treating skin disease in children with cancer:
- Children with melanoma may present with different clinical characteristics than adults. They are more likely to present as amelanotic, rapidly growing nodules. Incorporate modified diagnostic criteria for pediatric melanoma and consider the evolution of a lesion. Pediatric melanoma is rare but often diagnosed too late.
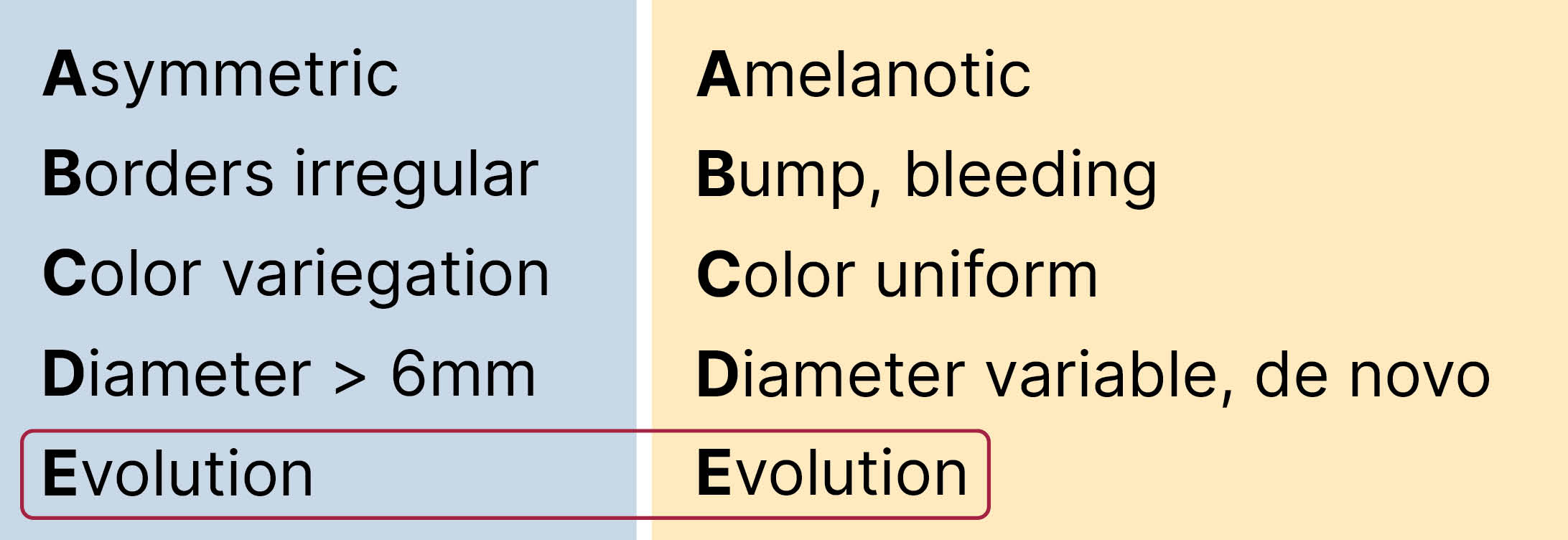
Tip #1: Children with melanoma are more likely than adults to present with amelanotic rapidly growing nodules.
- Perform BRAF V600E testing in cutaneous Langerhans cell histiocytosis (LCH) to provide guidance for prognosis and treatment. The BRAF V600E mutation is associated with decreased treatment response and higher incidence of reactivation. BRAF inhibitors can be used to treat refractory LCH.

Tip #2: Perform BRAF V600E testing in cutaneous LCH to provide guidance for prognosis and treatment.
- Among others, eruptive nevi and eczematous dermatitis are common benign reactions in children on mitogen-activated protein kinase (MAPK) inhibitors. Nearly all children on MAPK inhibitors develop cutaneous reactions. Dermatologists can reassure patients and other clinicians about these skin changes.

Tip #3: Eruptive nevi and eczematous dermatitis are common benign reactions in children on MAPK inhibitors.
- When an immunosuppressed patient presents with an itchy acneiform eruption of the face and scalp, suspect and treat demodex folliculitis. Demodex folliculitis is a common skin condition in immunosuppressed children that occurs when immunosuppression is weaned.

Tip #4: In face/scalp acneiform eruptions of immunosuppressed, suspect and treat Demodex folliculitis.
- Perform touch prep, a bedside diagnostic tool, to facilitate early diagnosis and treatment of cutaneous fungal infections. Angio-invasive fungal infections are life threatening and progress quickly in cancer patients.

Tip #5: Perform touch prep to obtain rapid diagnosis of cutaneous fungal infection.
- Rely on clinical signs and symptoms to diagnose acute graft versus host disease (GvHD). A biopsy is only needed to rule out infection or malignancy. Acute GvHD occurs in 30% of children after hematopoietic stem cell transplant (HSCT).

Tip #6: Rely on clinical signs and symptoms to make the diagnosis of acute GVHD.
- Recommend close surveillance for visceral chronic GvHD in patients with nail pterygium or vitiligo after HSCT. Nail pterygium is associated with lung chronic GvHD and worse pulmonary function. Vitiligo is associated with skin and visceral chronic GvHD.

Tip #7: Recommend close surveillance for visceral cGVHD in patients with nail pterygium or vitiligo after HSCT.
- Conduct annual skin checks for children who have been exposed to radiation, are on prolonged immunosuppression, or are on voriconazole. Childhood cancer survivors are at increased risk for skin cancer. Radiation therapy for children younger than 10 years of age exponentially increases the risk of basal cell carcinoma.
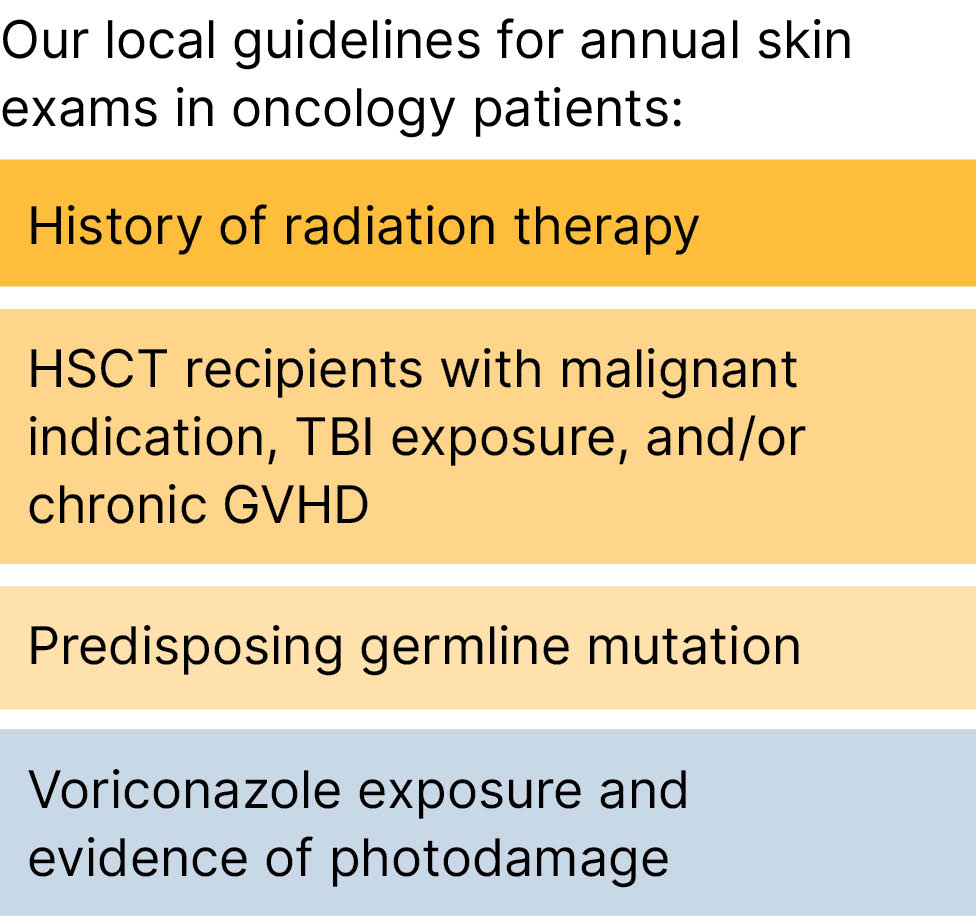
Tip #8: Annual skin checks for children exposed to radiation, prolonged immunosuppression and voriconazole use.
- Treat permanent chemotherapy-induced alopecia with oral minoxidil. Risk factors for permanent alopecia include radiation exposure, busulfan, and chronic GvHD. It is associated with depression, anxiety, and somatization in childhood cancer survivors. Many patients are not aware that treatment options exist.
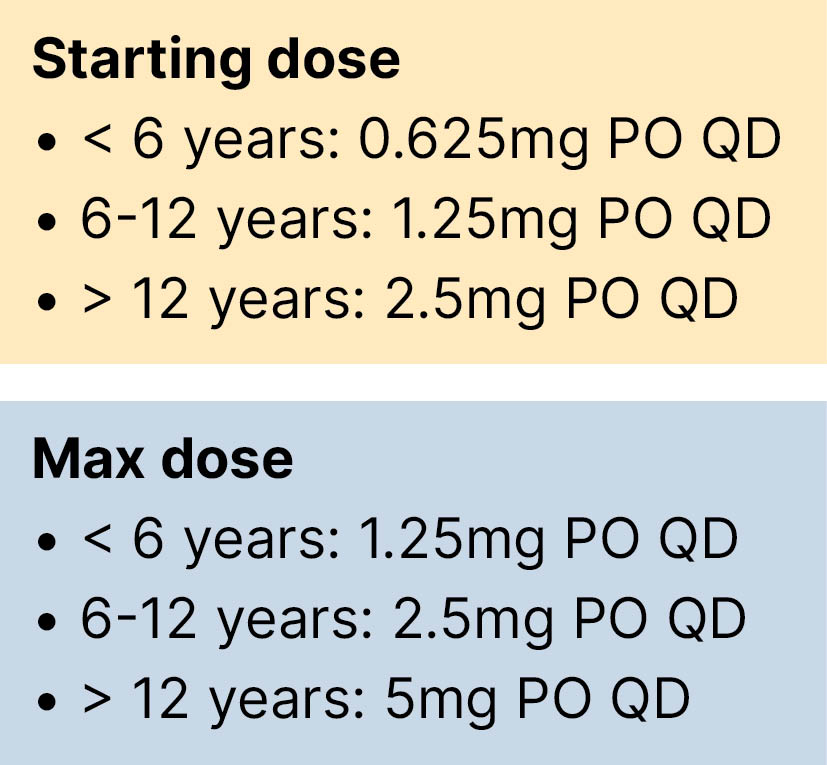
Tip #9: Treat permanent chemotherapy induced alopecia with oral minoxidil.
- Form an alliance with oncology colleagues by understanding their perspectives. Pediatric oncologists work closely with patients and families and appreciate communication about dermatologic care. Cancer relapse and infection are their top concerns when considering dermatologic treatment.
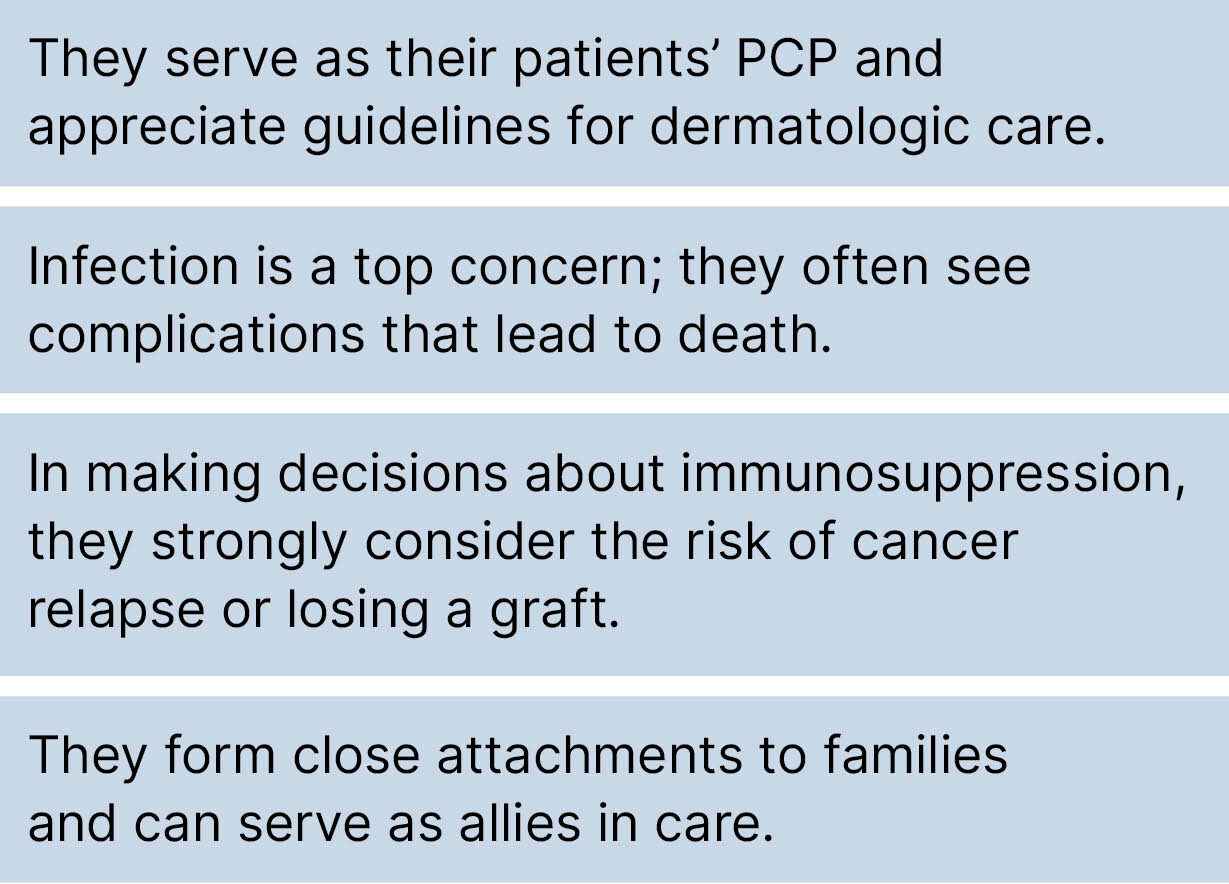
Tip #10: Form an alliance with your oncology colleagues by understanding their perspectives.

