Caring for the Patient with Cutaneous Immune-Related Events
Steven T. Chen, MD, MPH, MS-HPEd, Assistant Professor of Dermatology, Harvard Medical School, Vice Chief of Education, Department of Dermatology, Associate Program Director, MGH, Harvard Dermatology Residency Program Co-Director, Comprehensive Cutaneous Lymphoma Program, MGH Cancer Center
December 2022
Dr. Chen presented new research on the management of dermatologic immune-related adverse events (D-irAEs), including high-yield tips, and discussed potential future implications and therapeutic care of patients who receive immune checkpoint inhibitors (ICIs).
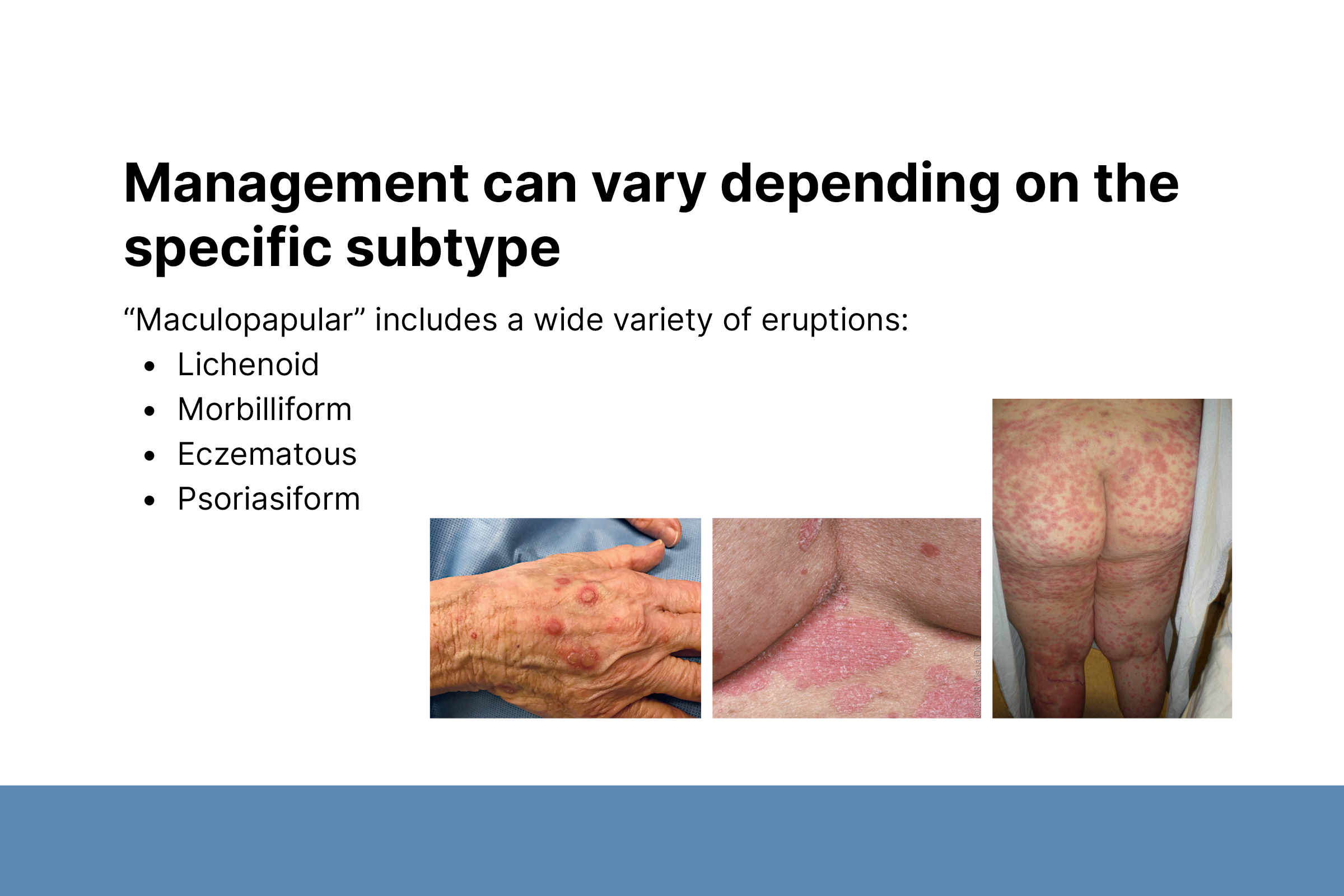
Dr. Chen shared his best ways to manage skin toxicity for patients with rashes who have discontinued ICIs. Management really depends on the subtype. He says “Personally, I would still exercise a little bit of caution before I jump to biologics because we don’t have a ton of data to show that it’s actually completely safe.” Dr. Chen respectfully disagrees with current guidelines recommending systemic steroids for Grade 2 adverse events, and he tries to avoid systemic steroid use. He talked about what he does instead, and how to think about steroid dosing, if necessary. He discussed alternative options for the treatment of grade 3 or 4 adverse events, such as tocilizumab or infliximab.
Dr. Chen talked about D-irAEs, specifically ICI-psoriasis, pruritus without rash, and lichenoid eruptions. He avoids systemic immunosuppression for these reactions, if possible. Before starting anything systemic, he consults with his oncology colleagues. Typically, targeted therapy will have better outcomes and is preferred over systemic immunosuppression (e.g., prednisone).
In summary, Dr. Chen’s take-home messages were that particular morphologies should prompt dermatologists to screen their patients for other potential irAEs. This may impact the treatment plan, which should include: partnering with the patient’s oncologist on systemic therapy decisions; avoiding immunosuppression, if possible; and when necessary, trying to limit the dose and duration of systemic steroid treatment or choosing a more targeted therapy approach.