Cancer Overdiagnosis: A Dermatopathologist’s Perspective
Daniel Bennett, MD, FAAD
Professor and Vice-Chair of Clinical Affairs, Department of Dermatology, University of Wisconsin – Madison, School of Medicine and Public Health
December 2023
Dr. Bennett shared his perspective on melanoma overdiagnosis and how to address the problem.
First, Dr. Bennett advised dermatologists to be careful about the language they use to describe melanoma screening and diagnosis. “Overdiagnosis” means using current diagnostic criteria to correctly diagnose a condition that may not harm the patient. Overdiagnosis does not mean misdiagnosis. “Screening” is a population-based intervention conducted in healthy, asymptomatic individuals with no risk factors for disease. When a patient sees the dermatologist because of abnormal lesions or history of skin disease, the appropriate term is “diagnostic examination.” Dr. Bennett prefers the terms “small tumor” or “lower-stage disease” rather than “early diagnosis.”
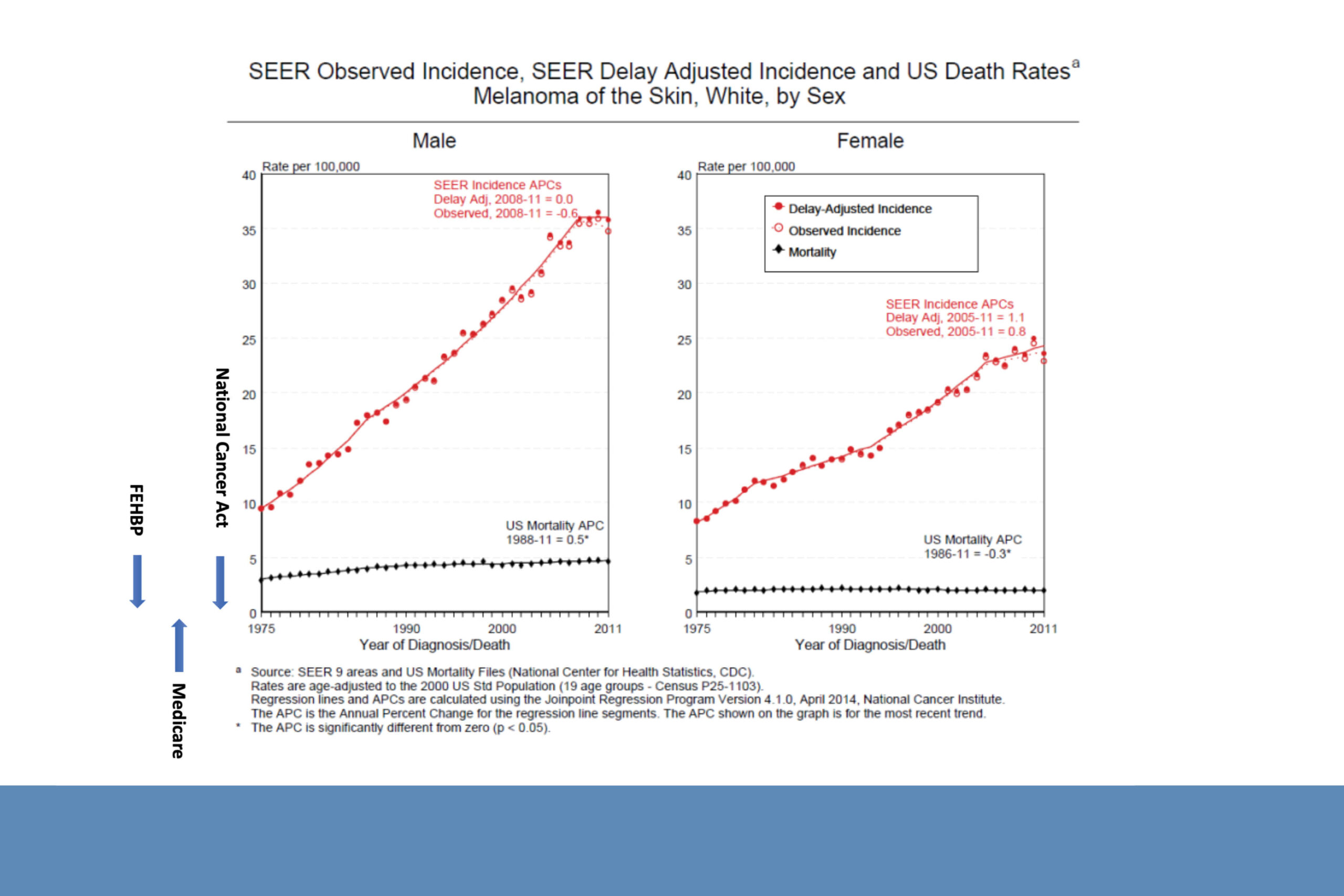
Second, Dr. Bennett argued that overdiagnosis is a cultural, social, economic, and political phenomenon caused by increasing awareness of cancer and expanding access to healthcare. Overdiagnosis is not a new issue and is not unique to melanoma. More tumors are identified because more patients are coming to dermatologists for skin concerns.
Melanoma overdiagnosis reflects the biology of the disease. Tumor behavior is complex and depends on characteristics of both the tumor and the host. Because it is difficult to predict which tumors will cause future progressive disease, each patient should be diagnosed and treated appropriately. Dr. Bennett emphasized that overdiagnosis is an epidemiological phenomenon occurring at the population level that cannot be applied to individual patients.
Dr. Bennett addressed other potential drivers of melanoma overdiagnosis including financial incentives and diagnostic drift. There are financial incentives in all fields of medicine to provide more treatment for patients than may be necessary. Diagnostic drift means that dermatopathologists today are more likely to diagnose melanoma in specimens that previously would have been labeled benign dysplastic nevi.
This occurs because it is more difficult to predict the future behavior of smaller tumors, resulting in increased diagnostic uncertainty. Dr. Bennett does not believe that financial incentives or diagnostic drift are driving the increasing incidence of melanoma.
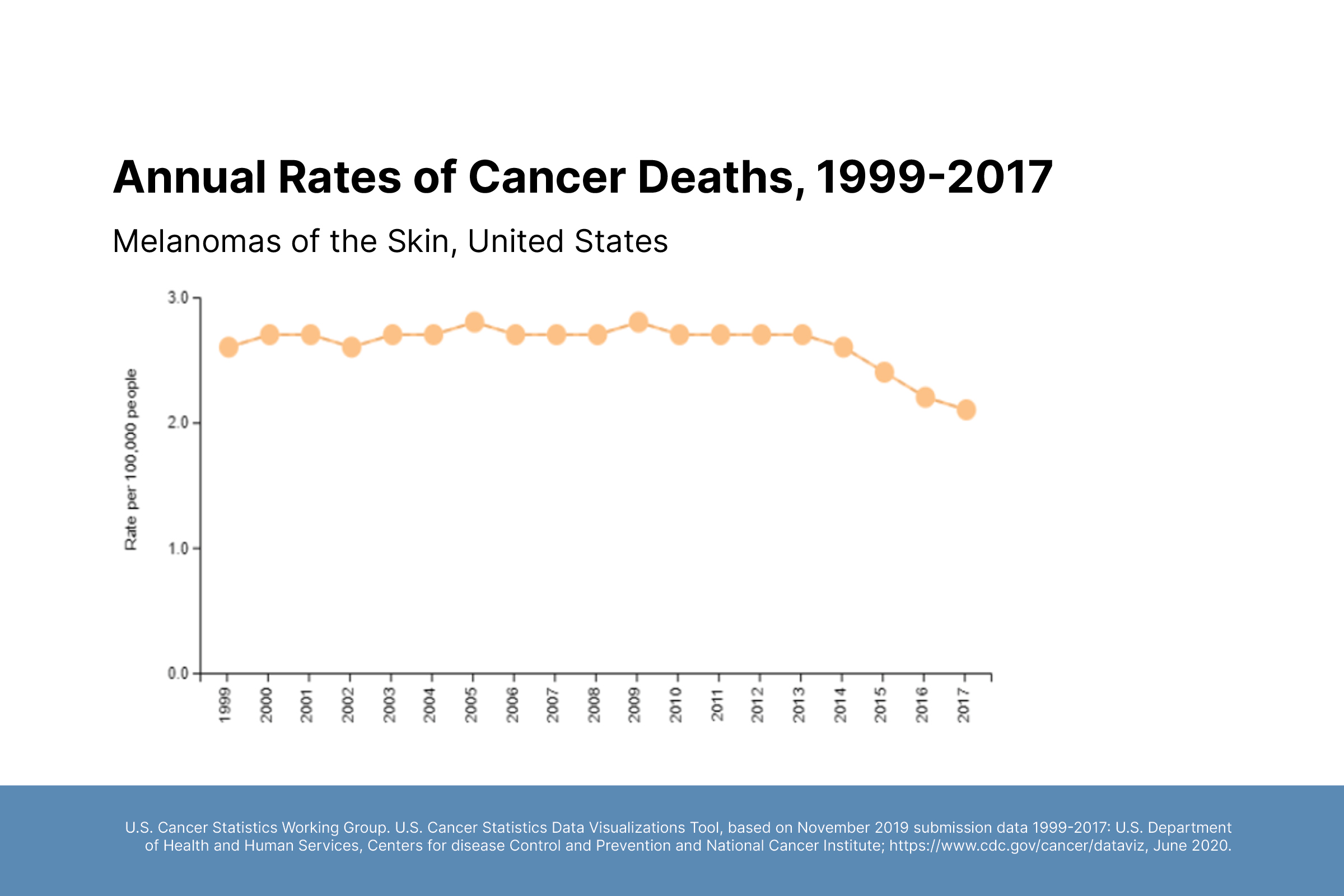
Finally, Dr. Bennett discussed interventions at the population level to address overdiagnosis. It is important to focus on outcomes that matter: reducing mortality and improving quality of life. There is currently no evidence that finding smaller tumors will save lives. Dr. Bennett believes that targeted melanoma screening in high-risk populations is most likely to provide benefit and may reduce the morbidity of keratinocyte carcinomas and mortality of squamous cell carcinoma.