Varicose Veins for Dermatologists
Ashley Wysong, MD, MS
Professor and Founding Chair, William W. Bruce, MD Distinguished Chair of Dermatology, Department of Dermatology, University of Nebraska Medical Center (UNMC)
June 2024
Dr. Wysong presented information about varicose veins for dermatologists. Dermatologists frequently see patients with venous disease in clinic but have limited formal training in treating it.
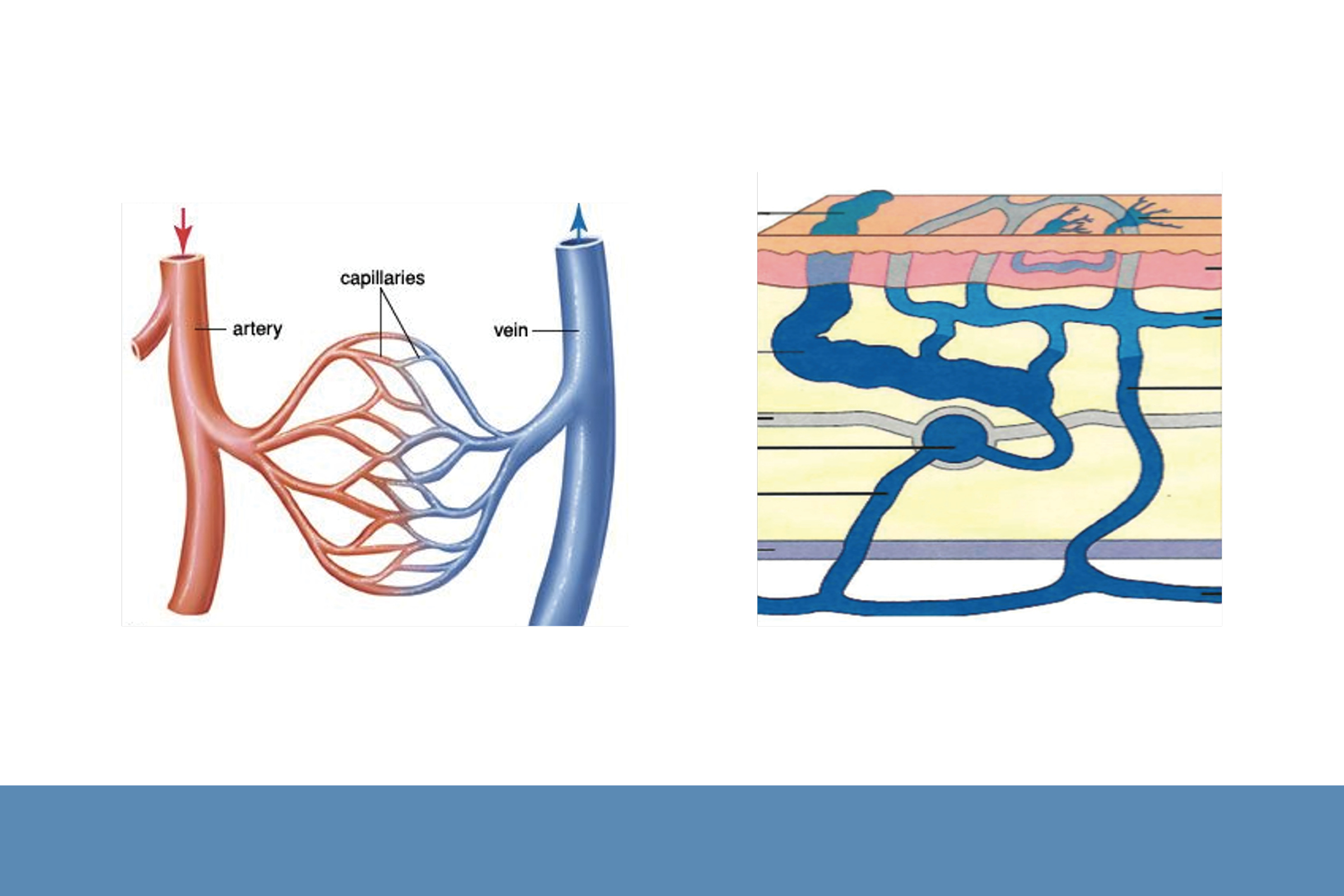
First, Dr. Wysong shared an overview of varicose vein disease including anatomy, epidemiology, pathophysiology, and clinical presentation. Venous insufficiency is the inability of the blood to return efficiently from the feet to the heart. It is usually a secondary process due to malfunctioning valves over time. Risk factors include age, genetics, exposure to hormonal therapies, number of pregnancies, and prolonged sitting or standing. Venous insufficiency is common and affects up to 55% of women and 45% of men.

Clinical presentation includes aching, tiredness, pain, or restlessness in the legs; lower extremity edema; and tenderness over the vein. Dr. Wysong cautioned that new-onset lower-extremity edema should be examined to rule out other causes including heart, liver, or kidney failure.
Second, Dr. Wysong described the clinical evaluation of venous insufficiency, including history and physical exam. She emphasized that all female patients should be asked about gynecological history and pelvic symptoms. Based on physical exam findings, venous insufficiency is classified from no signs of disease (C0) to open venous ulcers (C6). Venous patterning includes varicose, reticular, or telangiectasias (spider veins). Female patients with venous insufficiency or varicosity in the inguinal, gluteal, or vulvar areas require further pelvic imaging in conjunction with interventional radiology.
Third, Dr. Wysong discussed diagnosis and management of venous insufficiency. She recommended a detailed bilateral duplex ultrasound for all patients with symptoms of venous insufficiency or physical findings of concern regardless of symptoms. She emphasized that the bilateral duplex ultrasound describes the entire venous anatomy and is conducted by ultrasonographers specializing in venous disease.
Dr. Wysong recommended medical management, including exercise, elevation, and compression stockings for all patients with venous disease. She cautioned that arterial insufficiency must be ruled out and arterial pulses documented before prescribing compression stockings.
If patients fail medical management or have advanced-stage disease (open ulcer or active bleeding), Dr. Wysong recommended minimally invasive surgical treatment, and she described techniques such as thermal endovenous ablation, endovenous chemical ablation, and visual sclerotherapy.
To conclude, Dr. Wysong advised when to place referrals of patients to vein experts. Referrals should be made for all symptomatic patients; patients with active or healed venous ulcerations, skin changes, and extensive varicose veins or edema; and patients who fail sclerotherapy.

