Skin Cancer Syndrome: Update on Gorlin Syndrome
Elizabeth Magill Billingsley, MD
Professor of Dermatology, Mohs Surgery, Penn State University College of Medicine, Penn State Hershey Medical Center
June 2024
Dr. Billingsley presented information about the etiology, diagnosis, and treatment of Gorlin syndrome.
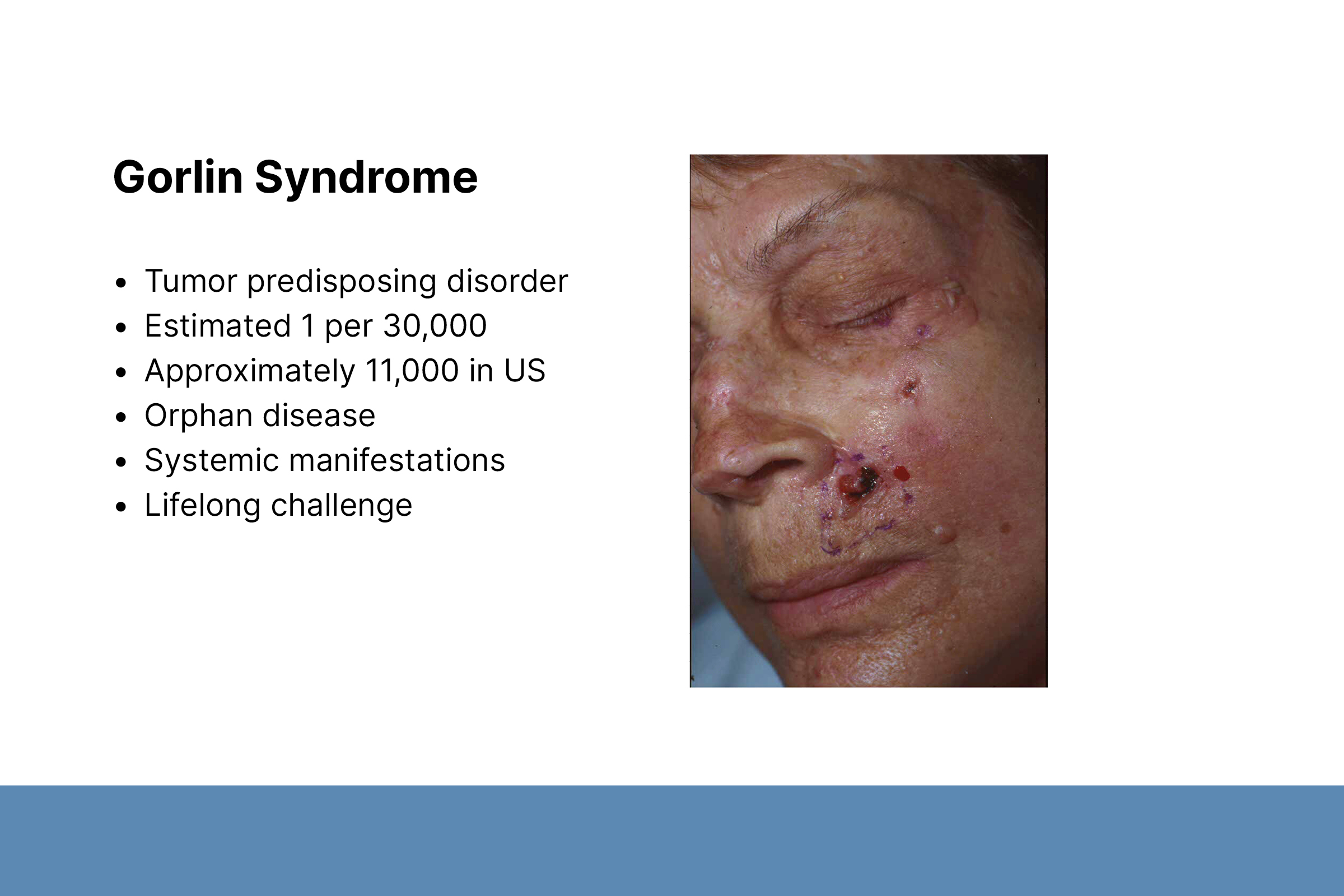
First, Dr. Billingsley discussed the etiology and epidemiology of Gorlin syndrome. Gorlin syndrome is a tumor predisposing disorder with systemic manifestations that affects approximately 11,000 people in the US. It is caused by a genetic mutation affecting the Sonic Hedgehog (SHH) signaling pathway. Most mutations occur in the protein patched homolog 1 (PTCH-1) gene but can also occur in PTCH-2, suppressor of fused homolog (SUFU), and other genes. Gorlin syndrome is autosomal dominant, and de novo mutations occur in 20–30% of cases. It occurs across ethnicities and genders.
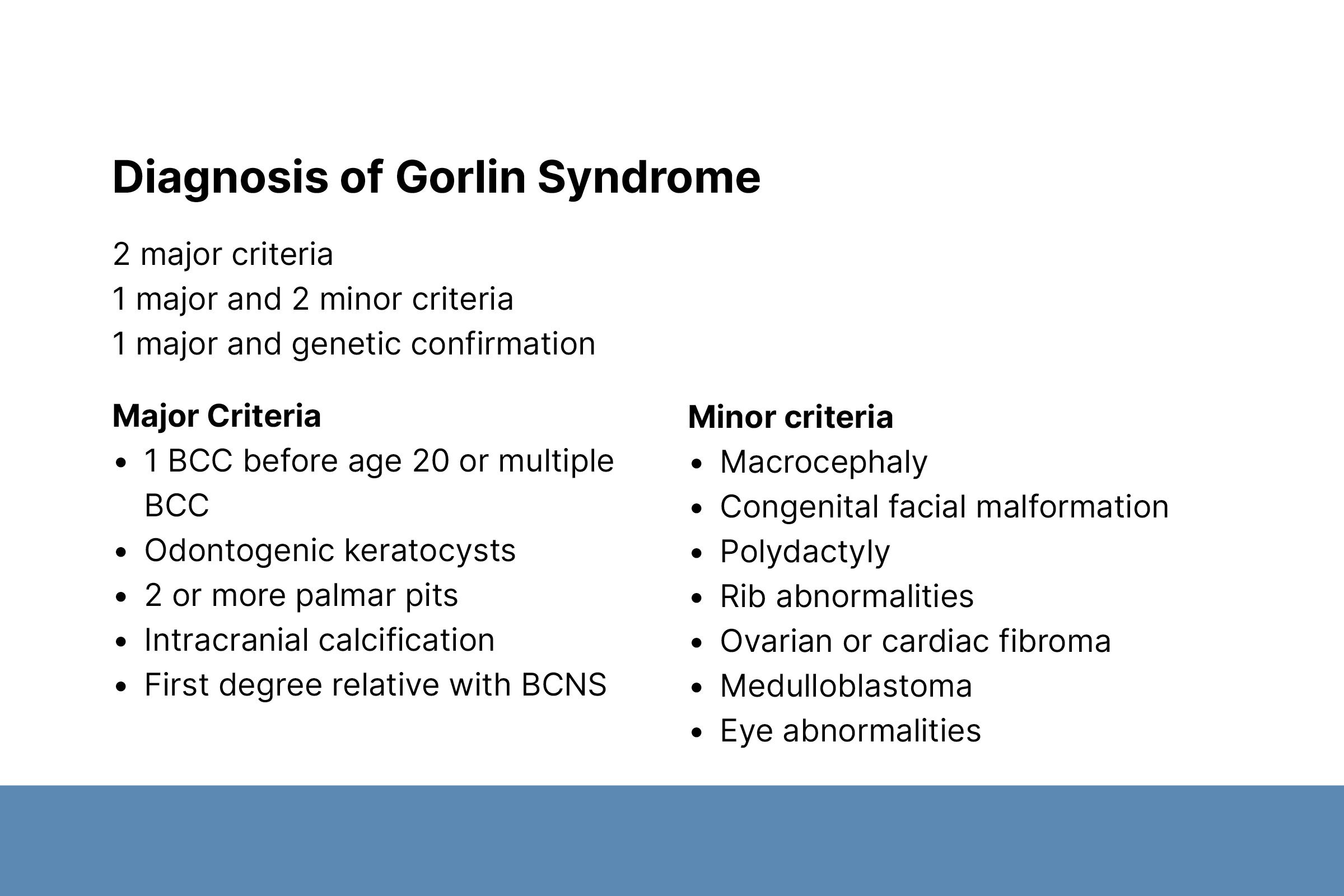
Second, Dr. Billingsley described Gorlin syndrome diagnosis, which is primarily based on clinical presentation. Major diagnostic criteria include 1 basal cell carcinoma (BCC) before age 20 years or multiple BCCs, odontogenic keratocysts, ≥2 palmar pits, intracranial calcification, and a first-degree relative with the syndrome. BCCs can occur in children 3–4 years old; the mean age is 25 years. BCCs do not appear in 10% of patients. Skeletal and facial abnormalities are common in Gorlin syndrome patients.
Third, Dr. Billingsley discussed Gorlin syndrome treatment and management. All patients need education about sun exposure and genetic counseling when considering having children. Treatment options for BCCs include surgery, topical creams, and systemic therapies. Surgical approaches include scissor tags, curettage, excision, and Mohs. Dr. Billingsley noted that Mohs should be reserved for specific situations such as recurrent tumors and tumors on the eyelid, lip, or ear, where preservation of normal skin is important. A balance must be struck among tissue preservation, higher cure rates, and surgical fatigue.
Topical creams imiquimod and 5-fluorouracil can be effective if patients can tolerate treatments. Side effects include skin discoloration, ulceration, increased sensitivity to sunlight, and pain and burning at the affected site.
Two oral SHH inhibitors are FDA approved for BCC: sonidegib for locally advanced disease and vismodegib for metastatic BCC. Dr. Billingsley recommended considering oral SHH inhibitors for patients who are surgically challenging; metastatic, otherwise inoperable, or poor surgical candidates; or have surgical fatigue. Like the topical creams, these oral SHH inhibitors can be effective but also can cause troublesome side effects including muscle cramps, fatigue, hair loss, and taste disturbance. Additional treatment options are niacinamide, laser treatment, and photodynamic therapy.
To conclude, Dr. Billingsley discussed the goals of treatment for Gorlin syndrome. She emphasized that treatment is multi-modal and personalized. The goal is not necessarily to eradicate all BCCs but to focus on the tumors that are most threatening, symptomatic, or bothersome to patients.

