Pediatric Connective Tissue Disease: Cases that Taught Me a Lesson
Yvonne E. Chiu, MD, Professor of Dermatology and Pediatrics, Vice Chair and Medical Director, Pediatric Dermatology, Medical College of Wisconsin
December 2022
Dr. Chiu presented 4 cases of pediatric connective tissue diseases and the lessons learned from each case.
In case #1, a 2.5-year-old boy presented with itchy papules on his knuckles and toes with no indication of muscle weakness on exam or laboratory work-up. Because of this, a study was done to review 46 cases of juvenile dermatomyositis (JDM). After work-up including MRI, only 2 cases were truly amyopathic with the only symptom being parent-reported fatigue. The lesson learned from this case is that JDM is difficult to detect, and a full work-up is required, including MRI and specific questioning about fatigue.
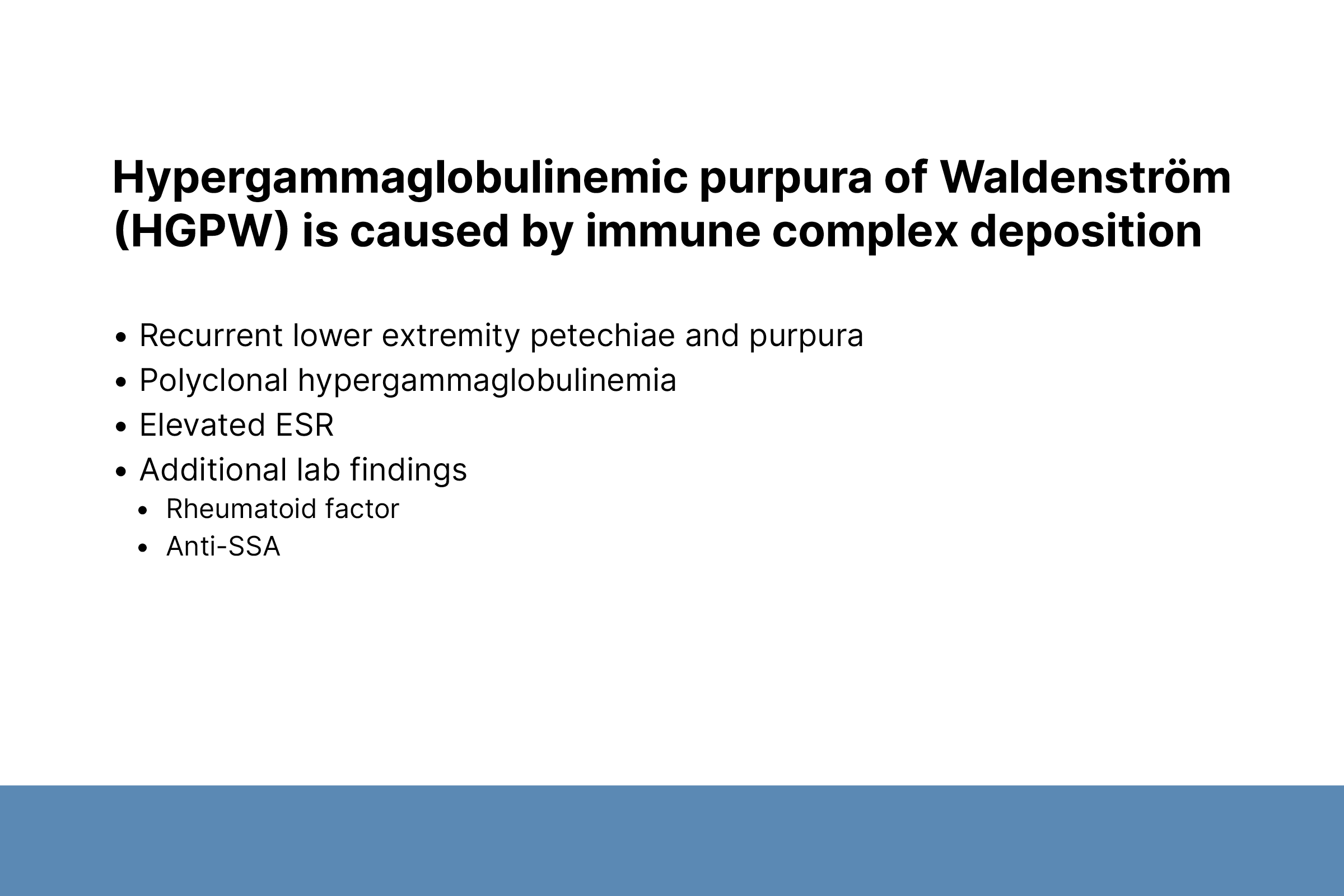
In case #2, a 16-year-old girl presented with recurring purpuric macules and patches on her lower extremities. She was diagnosed with primary sclerosing cholangitis at age 10, Crohn’s disease at age 13, autoimmune hepatitis at age 15, and eventually diagnosed with hyperglobulinemic purpura of Waldenström. The lesson learned is that hyperglobulinemic purpura of Waldenström is diagnosed by laboratory work-up and not histopathology because the histopathology of this disease is highly variable and nonspecific.
In case, #3, a 15-year-old boy with a history of donor engraftment after liver transplant presented with a rash of pink, scaly papules and plaques on his face. He was diagnosed with pediatric systemic lupus erythematosus, which likely occurred due to transfer of donor lymphoid cells that had developed a de novo genetic predisposition. The lesson learned is to be aware of autoimmune diseases occurring after solid organ and stem cell transplants, as these patients are at increased risk for developing secondary autoimmune diseases.
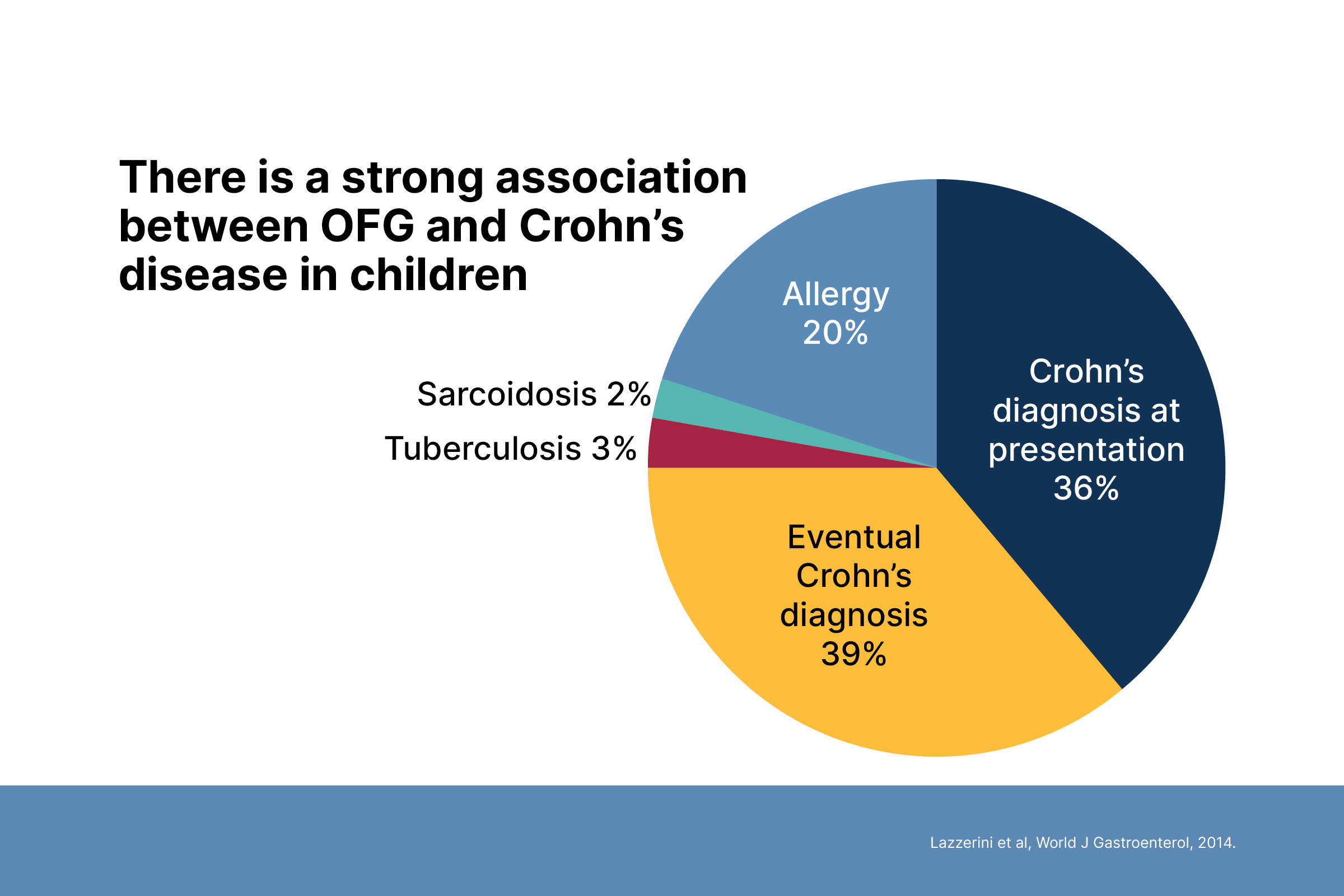
In case #4, an 11-year-old boy presented with swollen lips with no evidence of granulomas after 3 biopsies. Years later, he was eventually diagnosed with Crohn’s disease. The lesson learned here is to maintain a high index of suspicion for orofacial granulomatous and Crohn’s disease even without granulomas on biopsy.