How I Do It: Pediatric Psoriasis Cases
Yvonne E. Chiu, MD
Professor of Dermatology and Pediatrics and Vice Chair of Pediatric Dermatology, Medical College of Wisconsin
June 2024
Dr. Chiu presented information about the treatment of pediatric psoriasis beyond the use of topical steroids.
First, Dr. Chiu described treatment options for pediatric psoriasis when topical steroids are insufficient. When discussing treatment options with the family, she typically offers three categories: phototherapy, oral medication, and injectables. Dr. Chiu reads the room and uses parents’ reactions to guide the next steps.
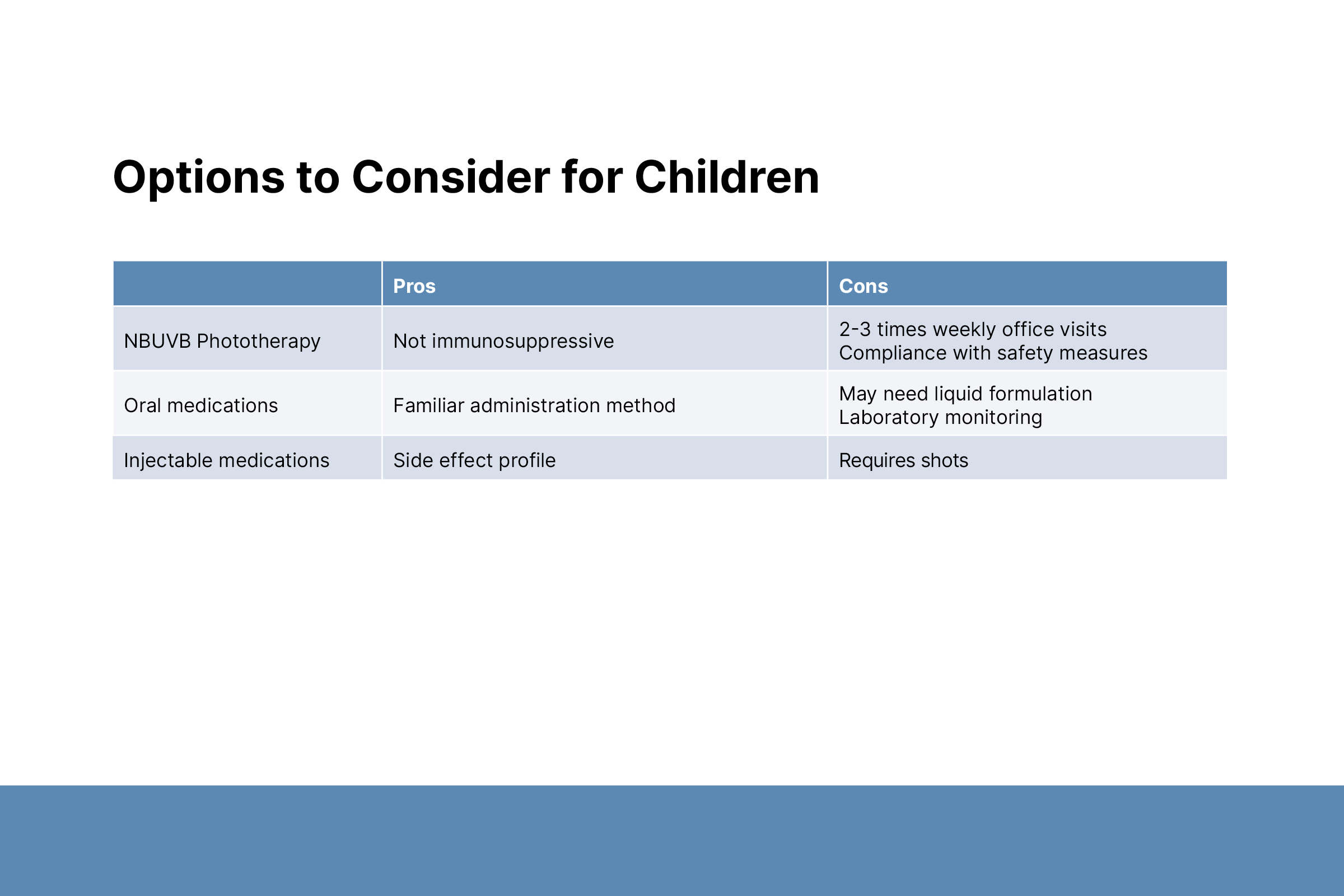
Narrow band UVB phototherapy is not immunosuppressive and has few side effects. Challenges of using UVB include the need for frequent clinic visits and patient compliance with safety measures. Dr. Chiu does not use phototherapy in patients younger than 5 years because of challenges with safety compliance.
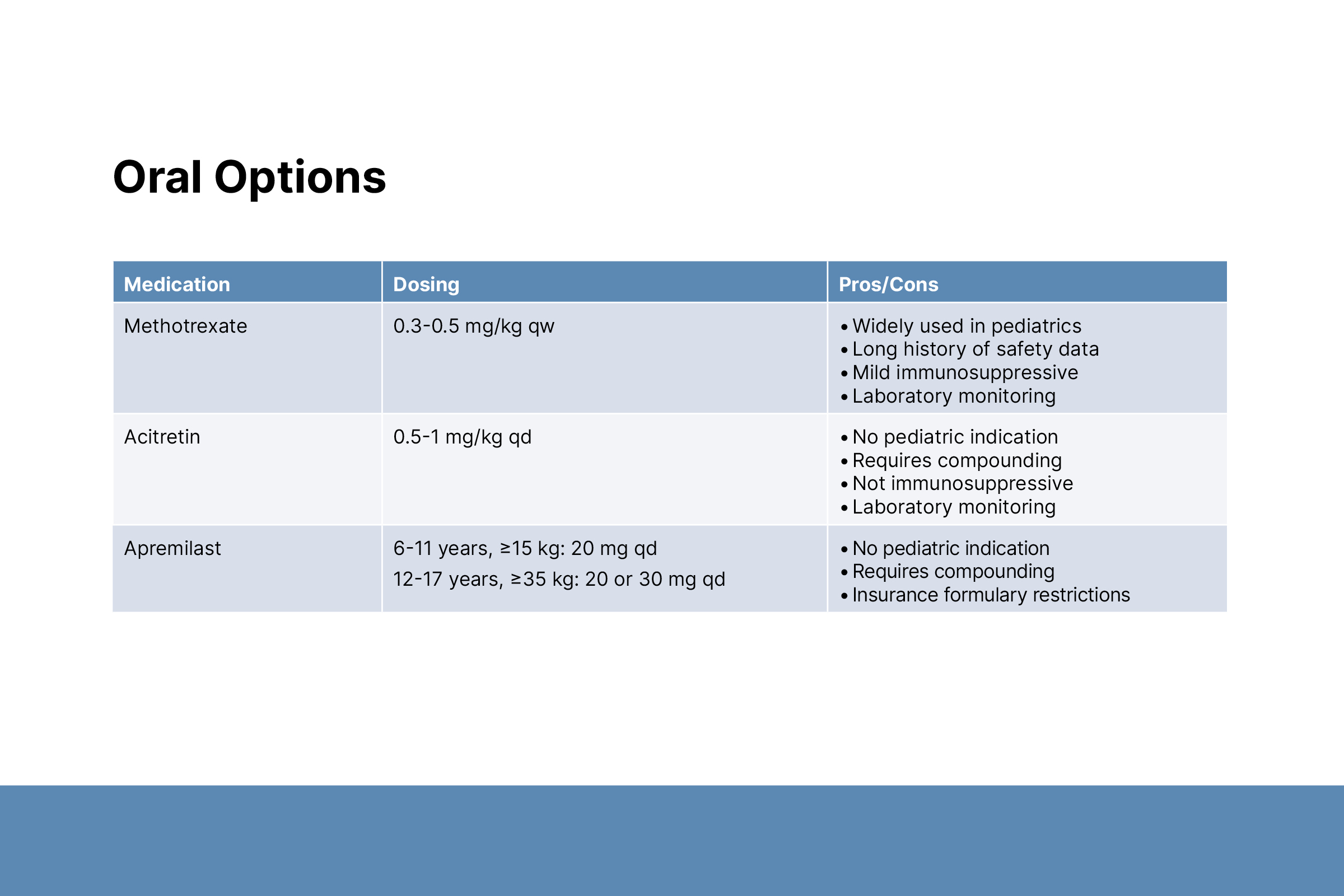
Oral medications include methotrexate, acitretin, and apremilast. Methotrexate is widely used in pediatrics.Acitretin and apremilast do not have pediatric indications, and liquid formulations must be compounded. Mild adverse effects of methotrexate commonly include stomach upset, fatigue, and headache. Subcutaneous methotrexate is preferred because it reduces the risk of stomach upset, but parents may be afraid of injecting their child at home. Side effects can be minimized with daily folic acid and Friday evening administration. Dr. Chiu advises families to mix methotrexate oral solution with orange juice to improve tolerability. Methotrexate laboratory monitoring is less rigorous in children. Labs should be checked at baseline, after one month of treatment, and every three months thereafter.
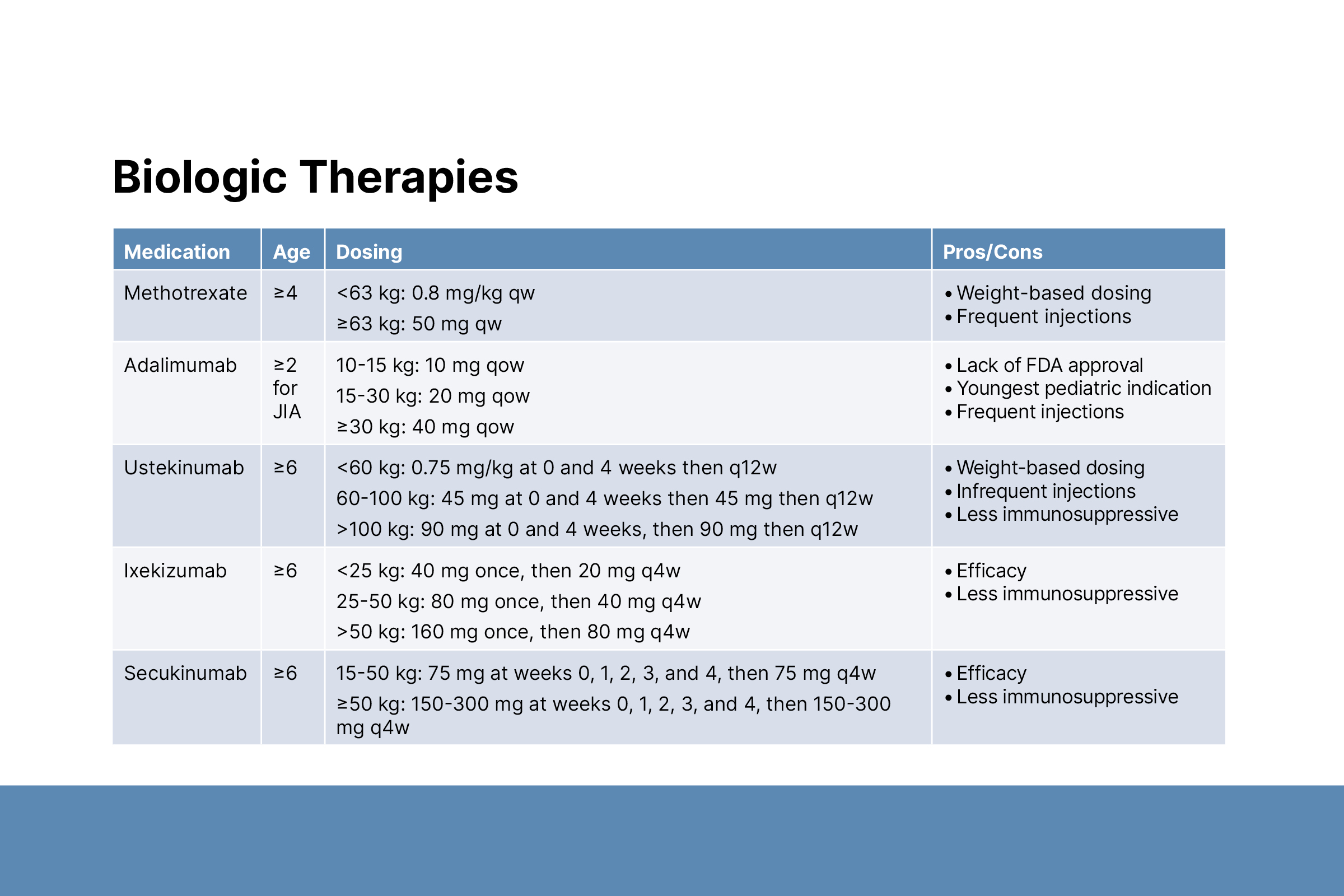
Second, Dr. Chiu discussed biologics. Biologics with pediatric indications include etanercept, adalimumab, ustekinumab, ixekizumab, and secukinumab. Dr. Chiu decides on a recommended biologic based on insurance coverage, step therapy requirements, injection frequency, and side effect profiles.
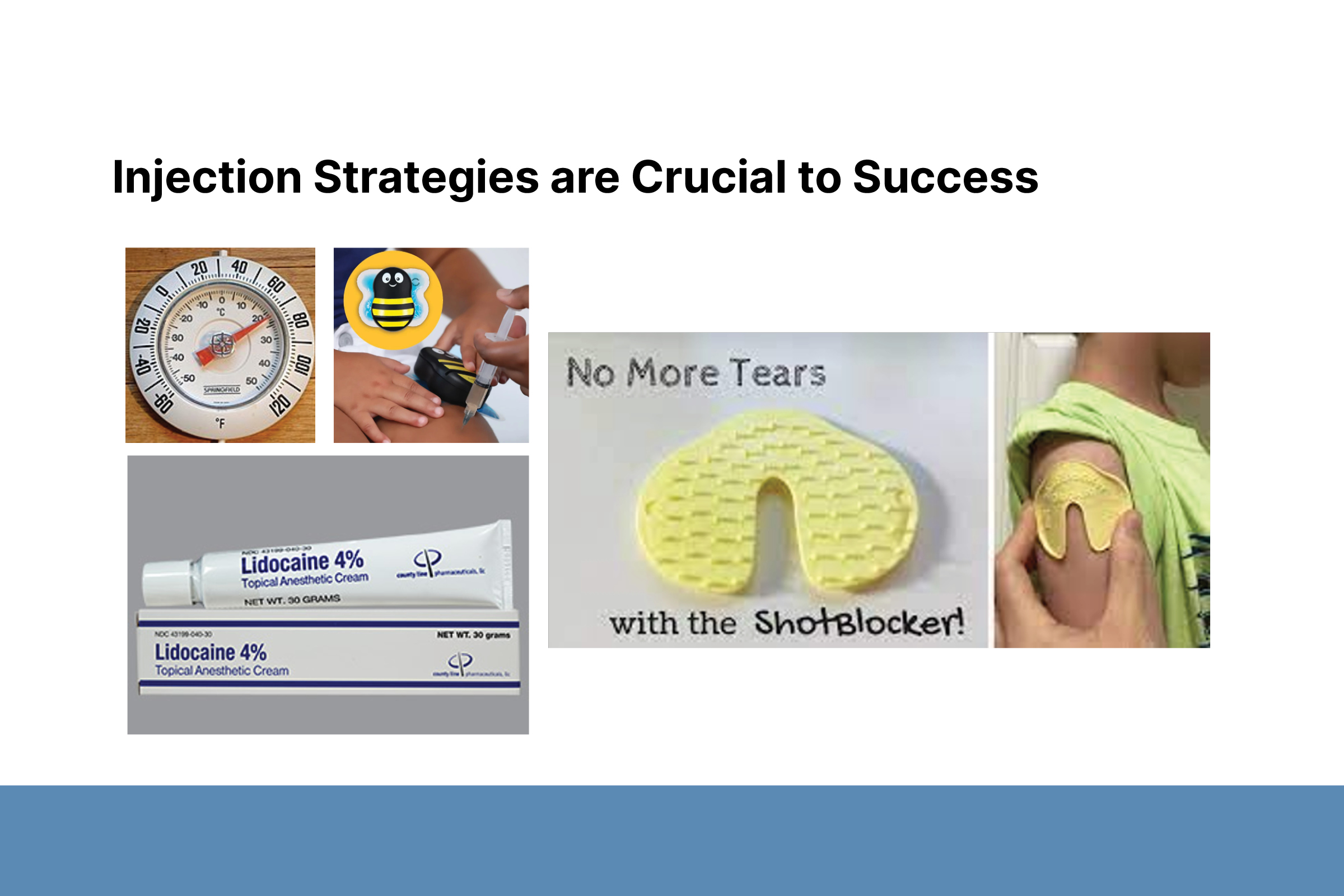
Dr. Chiu described injection strategies for success:
- The biologic should sit at room temperature before injecting.
- Apply topical lidocaine under occlusion (covered) 30 minutes before injecting.
- Distraction tools such as “Buzzy Bee” and “Shot blocker” may help.
- Choose the appropriate formulation. Injection pens hide the needle but have more force and must be discarded once deployed regardless of administration success. Syringes may be scarier but are sometimes preferable.
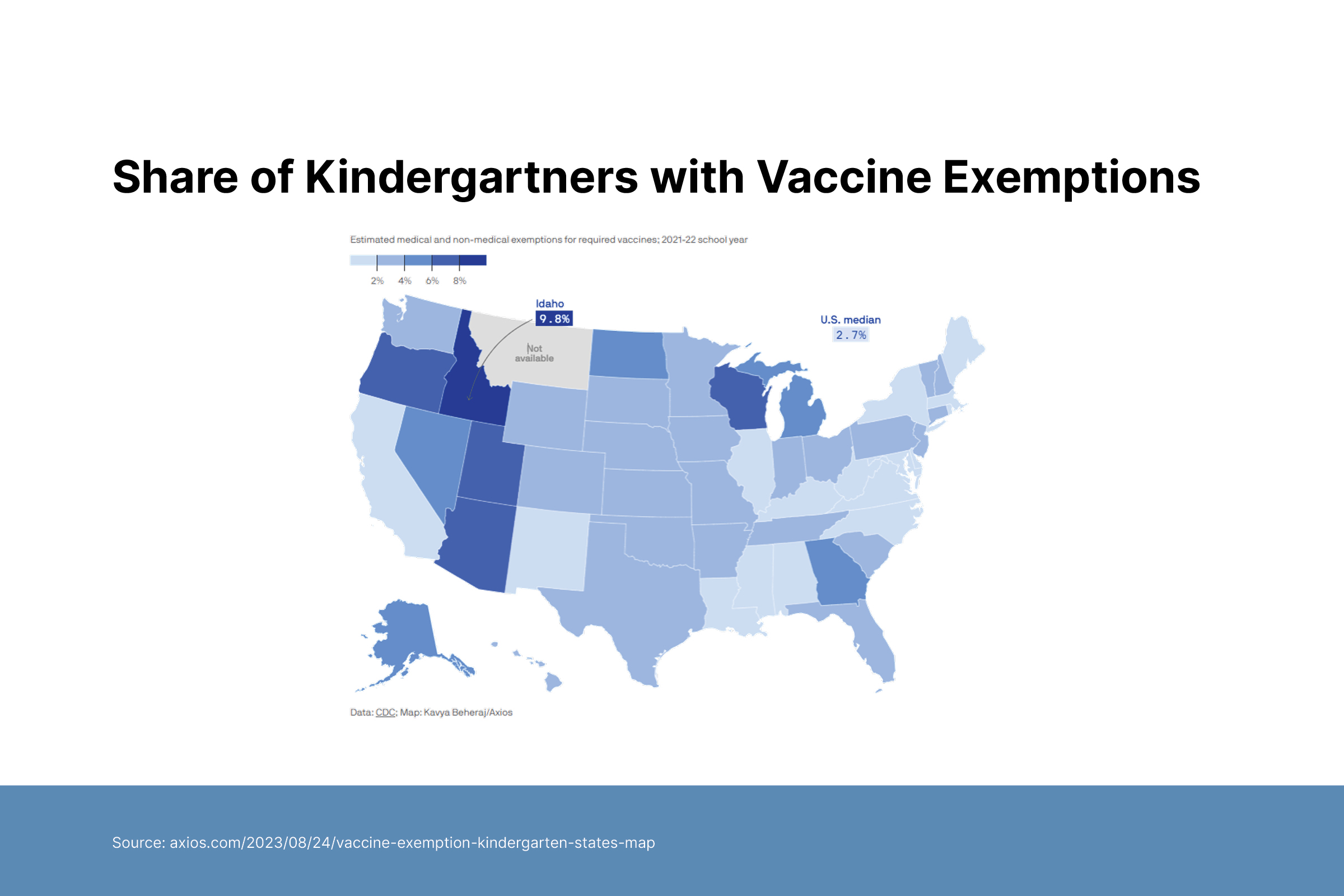
Third, Dr. Chiu shared vaccine management strategies for children on immunosuppressive biologics. Age-appropriate vaccines should be administered before starting immunosuppression. Non-live vaccines are safe to give during therapy. Immunosuppression must be paused if live vaccines are needed. Clinicians need to consider the risk of a disease flare versus the benefits of protecting a child from a potentially deadly infection. Shared decision-making among the dermatologist, pediatrician, and family is important.

