“From the Door” Diagnosis of Life-threatening Infections
Patient cases demonstrating the clinical presentation, diagnosis, and treatment of life-threatening cutaneous infections are sometimes referred to as “from the door” diagnoses.
October 2024
Dr. Lindy Fox presented four patient cases demonstrating the clinical presentation, diagnosis, and treatment of life-threatening cutaneous infections. She referred to these infections as “from the door” diagnoses because the clinical presentation is clearly concerning from the moment you walk in the door.
Case #1
A 33-year-old female with dermatomyositis presented with bullae and purpuric plaques, especially in the groin area. The patient was diagnosed with the angioinvasive infection ecthyma gangrenosum (EG).
EG classically presents as pink macules or papules that become nodules or hemorrhagic bullae and necrotic eschar. It commonly affects the perineal and gluteal areas and extremities. The predominant cause of EG is Pseudomonas aeruginosa. Other causes include non-Pseudomonas bacteria, non-tuberculous mycobacteria, and fungus.
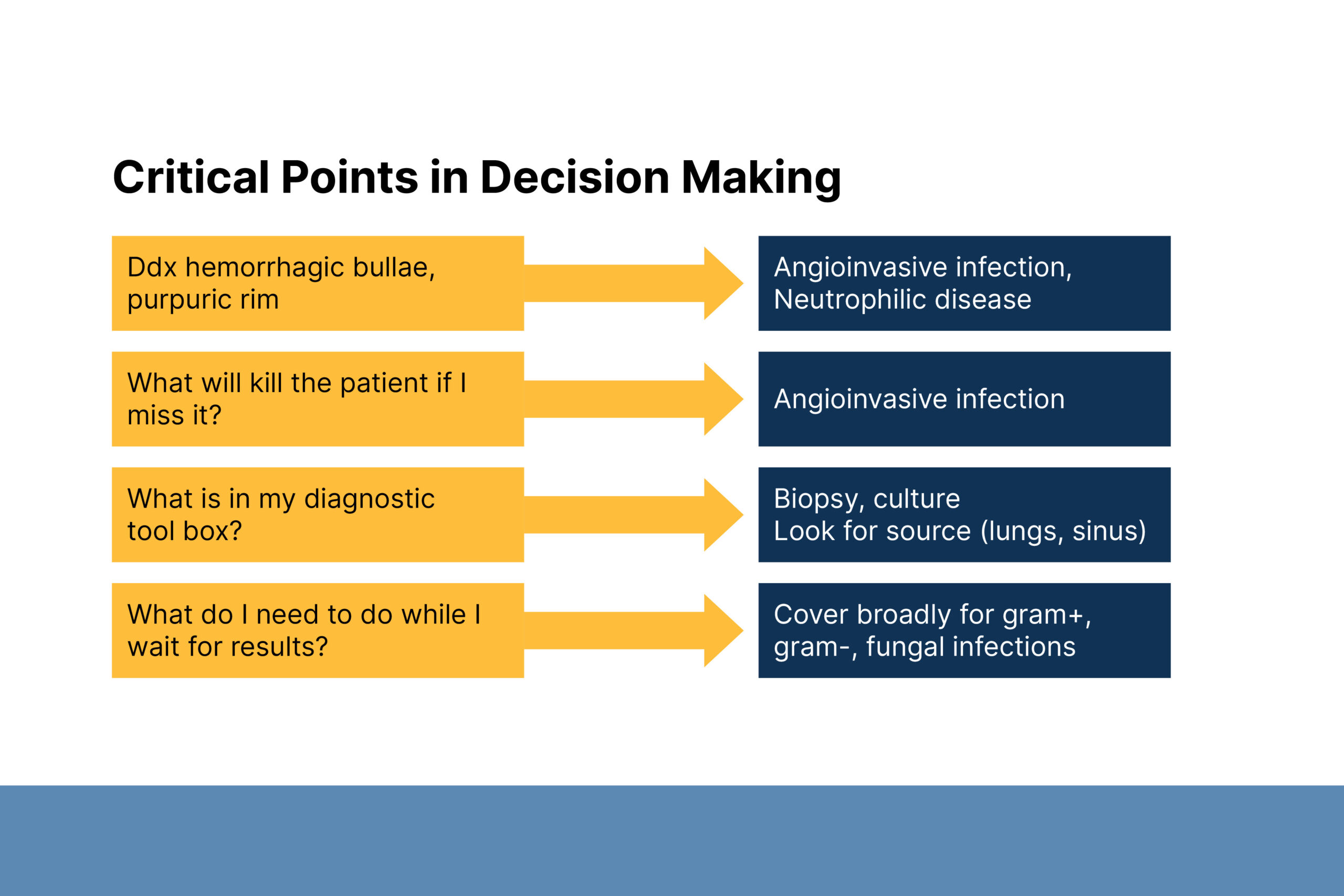
Dr. Fox emphasized that angioinvasive infections can be fatal. It is important to conduct a thorough workup of bacterial and fungal causes and treat them broadly while waiting for results. Fungal EG only occurs in immunocompromised patients. Bacterial EG occurs in both immunocompromised and immunocompetent patients.
Case #2
A 49-year-old male with multiple comorbidities presented with distal lesions characterized by hemorrhagic bullae, necrosis, and a purpuric rim. Lesion cultures showed Mucorales infection.
Invasive fungal disease is the leading cause of morbidity and mortality in immunosuppressed patients. Dr. Fox described current trends in invasive fungal infections. Antifungal resistance is increasing due to climate change, agricultural practices, and globalization.
Dr. Fox’s clinical pearls for diagnosing invasive fungal infections include:
- Infection from the lungs or sinuses is most likely to be Mucor or Aspergillus.
- Infection from the nails is more likely to be Fusarium
- A few larger lesions are more likely to be Mucor or Aspergillus
- Scattered smaller purpuric lesions are more likely to be Candida or Fusarium
Dr. Fox discussed treatment considerations for invasive fungal infections. There are multiple new therapies that target different areas of the fungal cell.
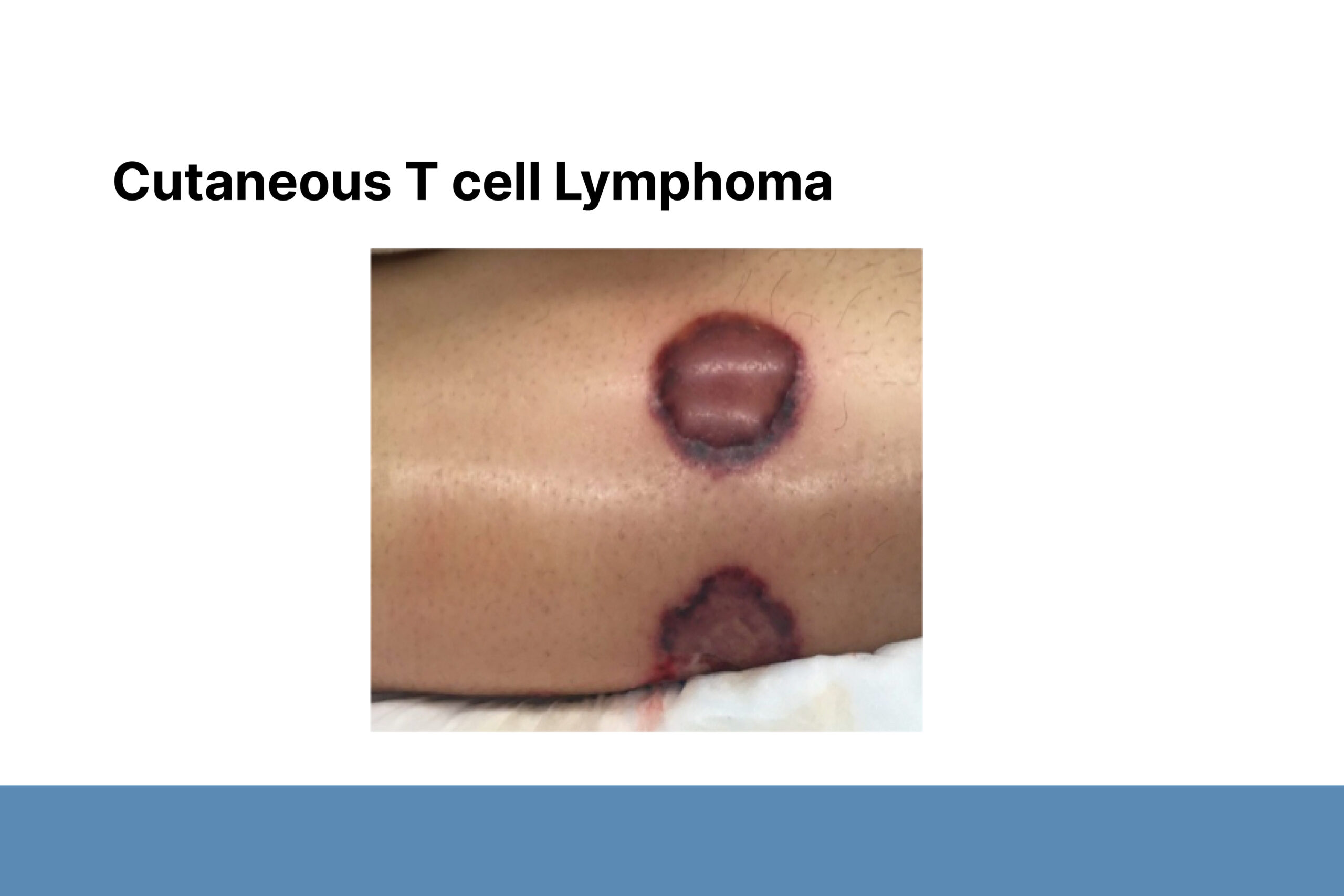
Case #3
A 29-year-old female with a liver transplant who was noncompliant with treatment presented with widespread cellulitic plaques and nodules. Cultures showed Cryptococcus infection.
Common morphologies of cryptococcal skin disease include cellulitis, subcutaneous nodules, and ulcers. Cellulitis is most common in organ transplant recipients. Molluscum-like lesions are most common in HIV patients. When cutaneous Cryptococcus is identified, you must also look for systemic disease. Dr. Fox described cryptococcoid sweet syndrome that mimics Cryptococcus on pathology.
Case #4
A 58-year-old female with a kidney transplant developed acute respiratory distress and could not be weaned off a ventilator. The patient was diagnosed with Strongyloidiasis hyperinfection based on periumbilical purpura. Strongyloidiasis hyperinfection can co-occur with colitis, polymicrobial sepsis, pneumonia, and meningitis; eosinophilia was not present.
Register today for the 2025 Clinical Symposium.

