Dr. Daniel Klufas presented information about deroofing for Hidradenitis Suppurativa (HS). Deroofing is a surgical procedure to remove the skin overlying a hidradenitis cavity.
First, Klufas provided an overview of HS and HS surgical management. HS affects approximately 1% of individuals in the Western world, and its prevalence is higher in women and African Americans. HS is an inflammatory dermatologic disease caused by follicular rupture and dermal seeding of intrafollicular contents, leading to tunnel formation. The disease burden is significant – HS is associated with a number of comorbidities, including cardiovascular disease, diabetes, metabolic syndrome, anxiety, and depression.
Historically, surgical management was the mainstay of treatment for HS. However, recent advances in medical therapies can delay architectural damage to the skin, thereby changing the role of surgery for patients with HS. Because the permanent tissue damage created by HS can cause progressive disease and subsequent flares, patients with Hurley stage II and III disease may be the optimal candidates for surgical management. Nevertheless, patients with all stages of disease may benefit from surgical interventions such as excisional surgery, lasers, botulinum toxin injections, and deroofing.
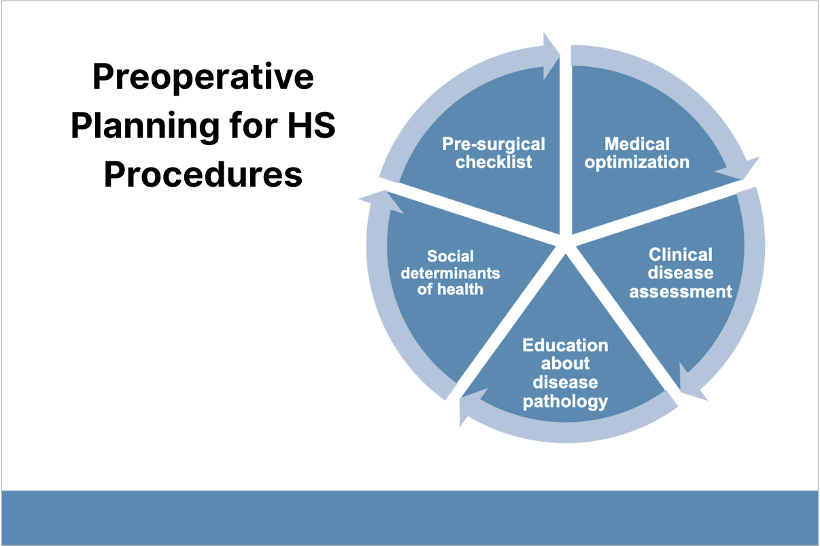
Pre-surgery consultation is key to understanding if someone is ready for the procedure and if expectations are clear and realistic.
Second, Klufas discussed patient selection for deroofing procedures. First, patients must be educated on the multifactorial pathophysiology of HS and understand that HS is a chronic condition that has no cure. This is important for setting patients’ expectations of surgical results. Additionally, candidates must be optimized with medical therapy, which is defined as treatment that prevents the development of new lesions in new locations. The best surgical targets for deroofing are symptomatic lesions that have recurred despite optimized medical therapy. Deroofing is not appropriate for patients with extensive Hurley Stage III disease affecting anatomically critical areas in the genitals or perianal location. Klufas shared patient cases to illustrate appropriate patient selection.
Third, Klufas described the deroofing procedure and shared surgical pearls:
- Ask patients where the site drains to identify the best opening to probe.
- Be sure to anesthetize widely, including the superficial and deep portion of the tunnel.
- Bevel the wound edges to prevent tunnel reformation.
- Debride the tract and remove the invasive proliferative gelatinous mass (IPGM). IPGM drives inflammation, leading to tract progression. Tracts will recur if IPGM is not sufficiently removed.
- Low-setting electrodessication at the periphery of the wound may prevent premature re-epithelialization.
Fourth, Klufas reviewed postoperative care and patient satisfaction. Wounds heal by second intent (without closure with sutures) in 2 to 8 weeks. Advantages of second intent healing includes smaller, cosmetically acceptable scars, an acceptable range of motion, no donor sites, no risk of flap or graft loss, and no activity restrictions. Patients should apply petrolatum to the wound and perform gentle debridement when bathing and changing dressings.
Deroofing has low morbidity and high patient satisfaction. Many patients report that HS flare pain is worse than postoperative pain. Klufas emphasized that medical therapy should continue after successful deroofing. Recurrence rates vary but are significantly reduced by concurrent medical therapy.
To conclude, Klufas described punch deroofing, which uses a punch biopsy tool to access and debride a small area. For patients in excruciating pain, punch deroofing can provide relief with improved recurrence rates compared to incision and drainage.
Mark January 28-31, 2026 on your calendar for the 2026 Annual DF Clinical Symposium.

