Clinic-Based Surgery for HS
Christopher J. Sayed, MD
Associate Professor of Dermatology, University of North Carolina at Chapel Hill
December 2023
Dr. Sayed presented information about clinic-based surgical procedures for patients with hidradenitis suppurativa (HS).
First, Dr. Sayed discussed the role of dermatologists in providing surgical care for HS. HS medications can be used to treat inflammation, but the physical wounds and skin changes remain. Surgery may be a good option for patients who do not improve with medications or for recurring wounds in the same location.
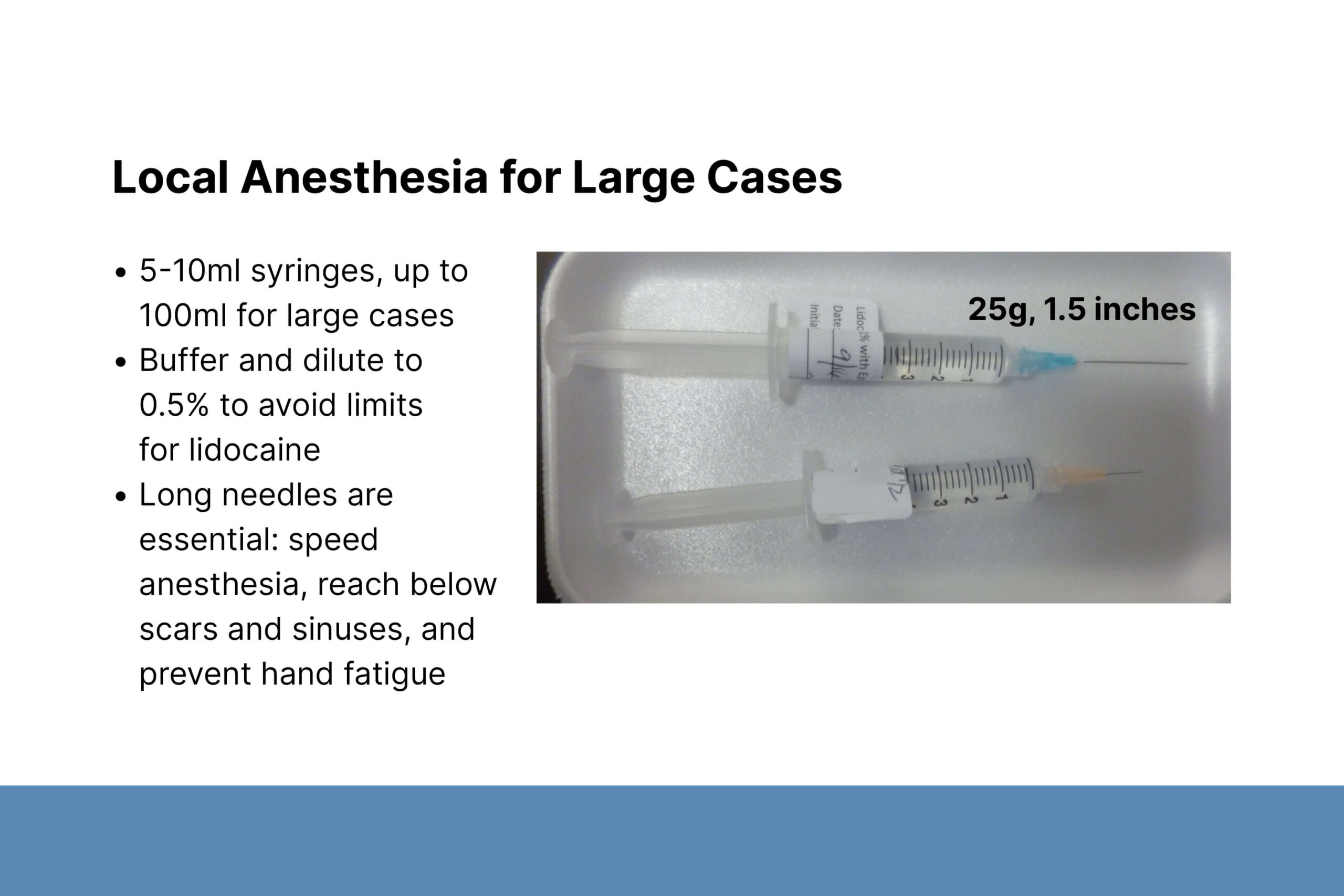
Dermatologists are skilled skin surgeons and can apply their expertise to HS wounds. Clinic-based surgery provides surgical treatment that is more accessible for many patients. Dr. Sayed began performing surgical procedures at the request of patients who were ineligible for general surgery due to comorbidities. Staging procedures can expand what is treated in the clinic. Wound size, anesthesia dosing requirements, and a patient’s tolerance for local anesthesia may limit clinic-based surgical treatment. Patients who prefer general anesthesia can be referred to general or plastic surgery.
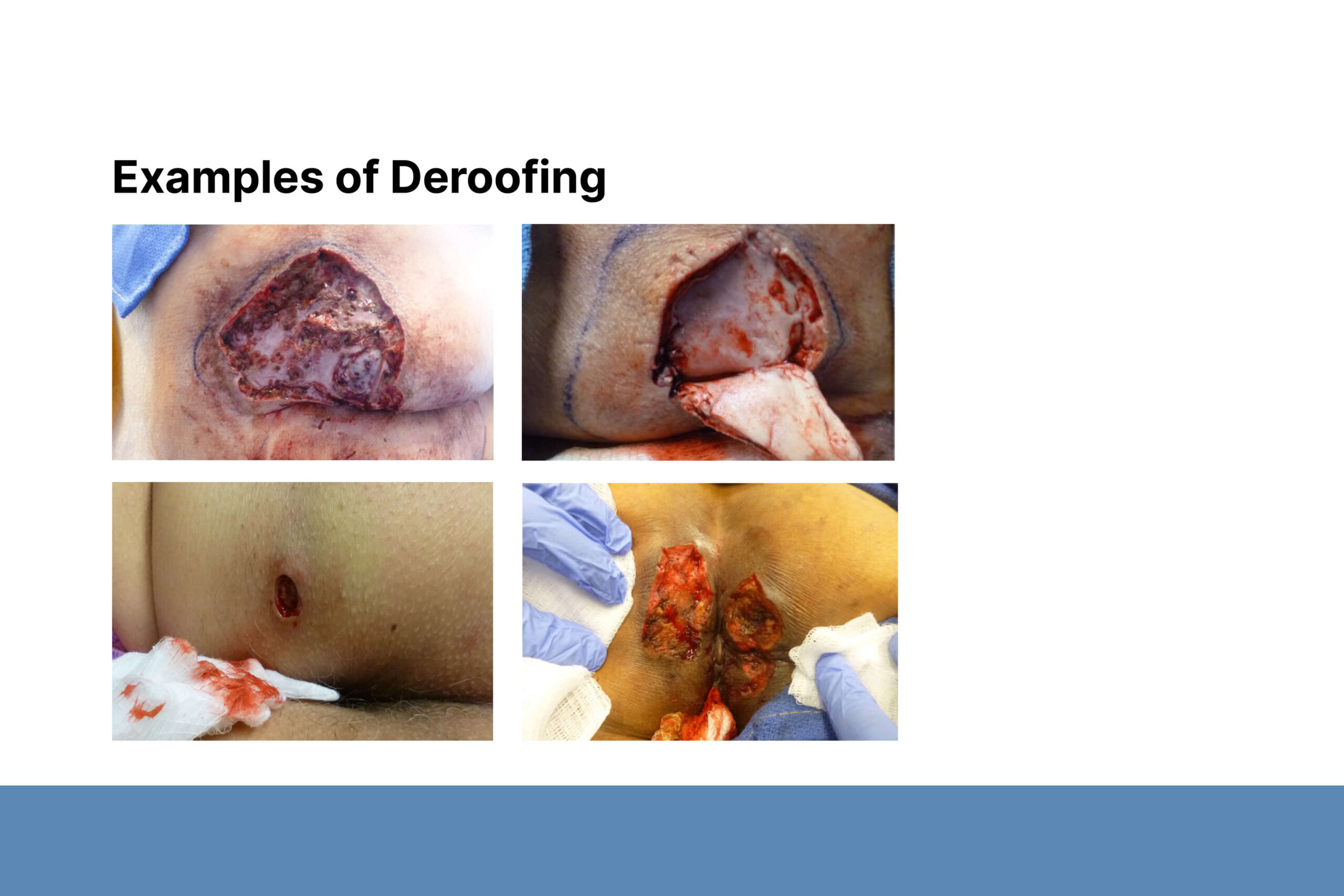
Second, Dr. Sayed described deroofing and excisional procedures. Before surgery, he marks the lesion based on palpation and confirms the location with the patient. He uses a fistula probe to identify areas of diseased tissue, which is mostly contained within the dermis. Wounds may ooze, but larger blood vessels should not be involved. Dr. Sayed emphasized the importance of continuing to probe the edges of an open wound to find all areas of disease. Diseased tissue that is not removed during surgery may cause recurrence and require additional procedures.
Post-surgical wounds often do not require sutures, especially larger wounds and wounds that extend over a joint. If patients strongly prefer sutured closures they may need to restrict physical activity longer. For high-tension wounds, Dr. Sayed places approximating sutures in the subcutaneous fat to take tension off the dermis prior to placing dermal and superficial sutures.
Finally, Dr. Sayed shared the experience of HS patients treated with surgery. When asked to compare the pain of a typical HS flare to post-surgical pain, 70% of patients reported that post-surgical pain is less than that of an HS flare. Because HS is characterized by chronic, non-healing wounds, creating a surgical wound that heals after a finite amount of time feels like success for patients. Dr. Sayed encouraged dermatologists to consider clinic-based surgery for their HS patients. There is a growing number of HS specialty clinics that can help.