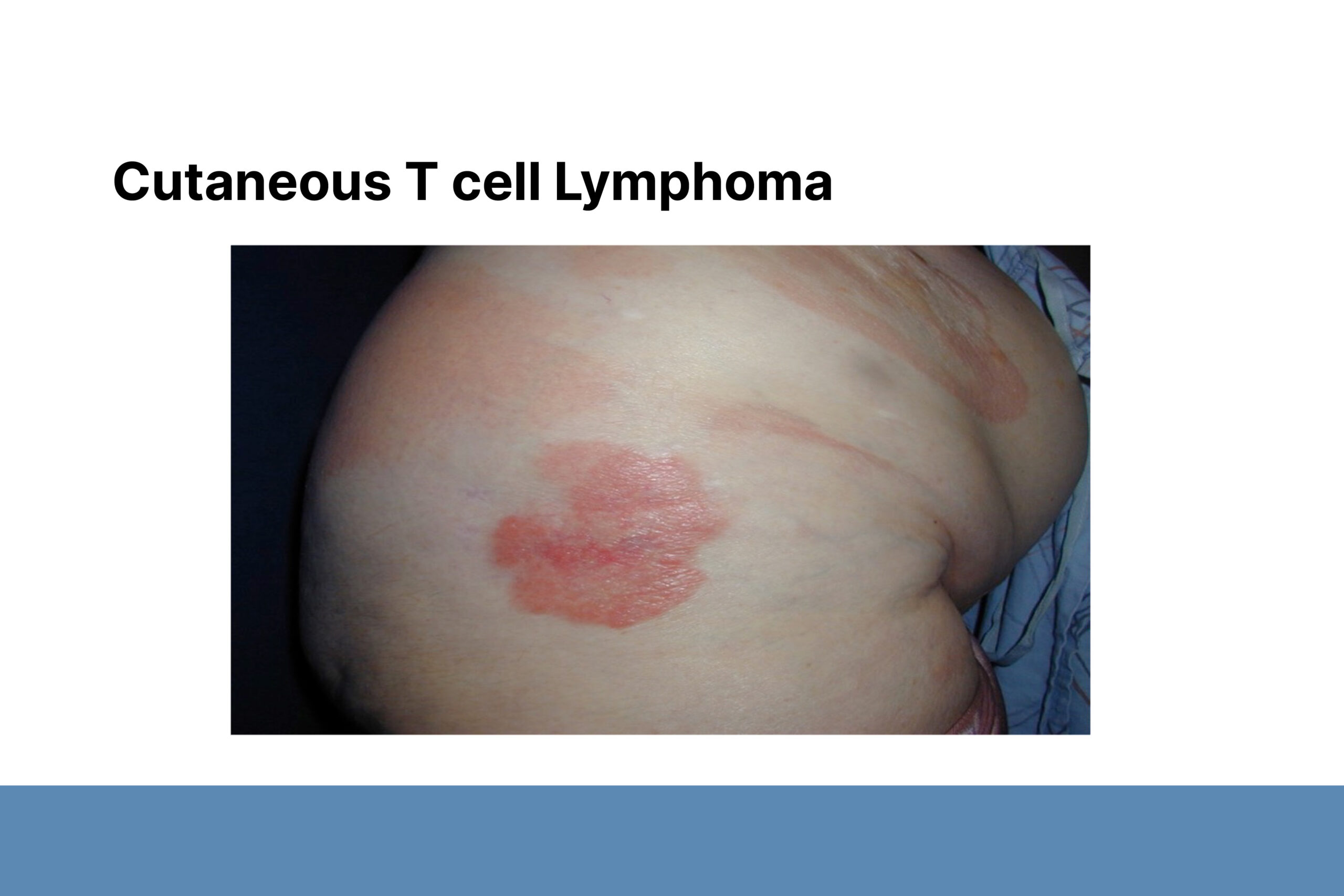
Can We Cure Cutaneous Lymphomas in 2024?
Analyzing patient samples using omics, machine learning, and AI helps identify therapeutic targets for further evaluation in clinical trials.
Dr. Jaehyuk Choi, PhD, Jack W. Graffin Professor, Associate Professor of Dermatology, and Biochemistry and Molecular Genetics, Northwestern University
October 2024
Dr. Jaehyuk Choi presented his research about novel therapies for cutaneous lymphomas. In his research, Dr. Choi analyzes patient samples using omics, machine learning, and AI to identify therapeutic targets for further evaluation in clinical trials. Dr. Choi shared three patient cases where he helped the treating physician find therapies to induce remission.
Case #1
An 80-year-old female with primary cutaneous gamma delta T-cell lymphoma (PCGDTL) on the head and face and no internal disease. The patient had multiple comorbid conditions, was ineligible for a bone marrow transplant, and had no other treatment options.
Biopsy sequencing identified a mutation in SOCS1, which inhibits Janus kinases (JAK) and suppresses the Janus kinase-signal transducers and activators of transcription (JAK-STAT) pathway. Immunohistochemical analysis revealed molecular upregulation of the JAK-STAT pathway. The patient was treated with the JAK1/2 inhibitor ruxolitinib and showed near clinical remission. Subsequently, the patient developed new mutations suggesting JAK inhibitor resistance and relapsed. Although the patient died, this case was the first time any treatment had been effective for malignant disease.
Case #2
A 74-year-old female with PCGDTL on lower legs and inguinal lymphadenopathy resistant to chemotherapy. Biopsy sequencing identified a JAK3 mutation. Treatment with the JAK1/3 inhibitor cerdulatinib led to near complete remission, but the patient subsequently relapsed. Analysis of new lesions showed novel JAK3 mutations.
In both cases, JAK inhibitors suppressed the disease but caused subsequent mutations that were resistant to therapy. Dr. Choi sees these results as opportunities to learn about cutaneous lymphomas and leverage knowledge about other cancers to find treatment combinations that can be effective longer term.
Case #3
A 13-year-old female with primary cutaneous aggressive epidermotropic T-cell lymphoma (PCAETCL). Analysis revealed a novel SATB1-FGFR1 gene fusion mutation. Treatment with pemigatinib, an FDA-approved SATB1-FGFR1 inhibitor, led to clinical remission but subsequent relapse. Further analysis showed novel mutations in FGFR1 predicted to mediate resistance to FGFR1 inhibitors. Researchers hope the patient can receive a stem cell transplant, in part because of induced remission.
Dr. Choi believes improved treatments and eventual cures derived from patient data are possible for PCGDTL, PCAETCL, and other aggressive cutaneous lymphomas.
To conclude, Dr. Choi discussed mycosis fungoides and sezary syndrome (MF/SS), the most common form of cutaneous lymphoma. Available treatments enable MF/SS patients to survive for many years. They are not cured, because they will relapse if they stop treatment or become immunosuppressed. However, Dr. Choi believes these patients can have longer lives with better quality of life without killing every cancer cell.

Register today for the 2025 DF Clinical Symposium.

