Big Medicines for Little People: Systemic Therapies in Pediatric Dermatology
Brittany G. Craiglow, MD
Associate Professor Adjunct, Dermatology, Yale School of Medicine
December 2023
Dr. Craiglow discussed systemic therapies for pediatric atopic dermatitis (AD) and psoriasis and shared tips for treating children.
First, Dr. Craiglow emphasized the importance of patient experience in assessing the severity of disease. She suggested asking patients how much the disease affects their life on a scale from 0 (not at all) to 10 (ruins my life). Even if the disease appears to be mild to the clinician, it could have a significant impact for the patient.
Quality of life is an important factor when considering systemic treatment for children. Clinicians must weigh the risks of treatment against the consequences of not treating. Dr. Craiglow shared the “7 Ss” of quality of life in children: self-esteem, social interactions, school performance, sleep, stigma, sustainability of topical treatment regimen, and involvement of special sites like the scalp or genitals.
Second, Dr. Craiglow described two FDA-approved systemic treatments for pediatric AD: dupilumab and upadacitinib. She considers dupilumab when patients report that the condition affects their life with a score ≥4, or if patients have comorbidities like asthma or eosinophilic esophagitis. Dr. Craiglow stated that needles are usually not a dealbreaker for systemic pediatric treatment and shared tips for administering injections in children.
Dr. Craiglow uses upadacitinib, an oral JAK inhibitor, for patients who do not respond to dupilimab, cannot tolerate injections, or have comorbid diseases like alopecia areata and vitiligo that could benefit from JAK inhibitors. One notable side effect of upadacitinib is acne; management is the same as acne in general.
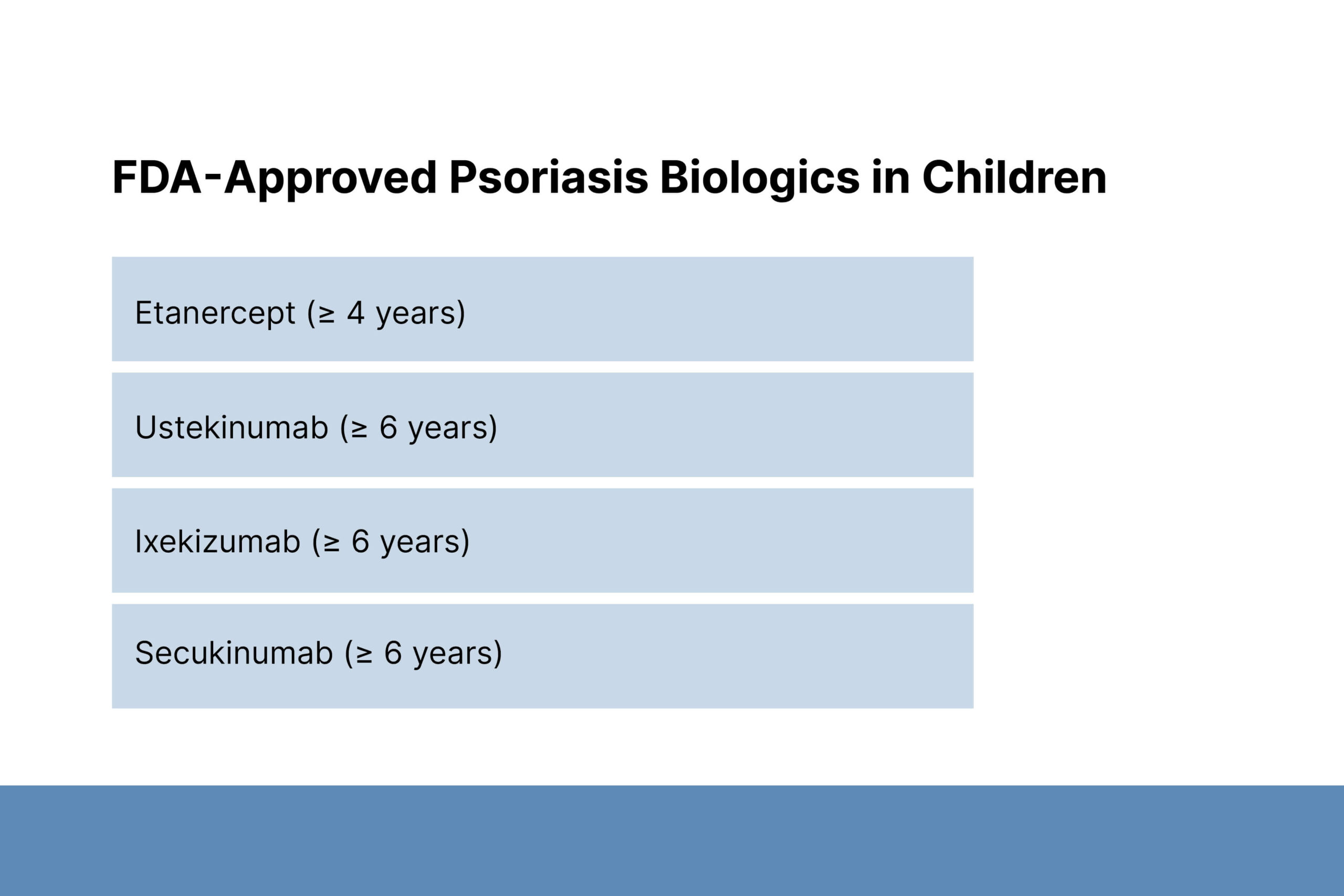
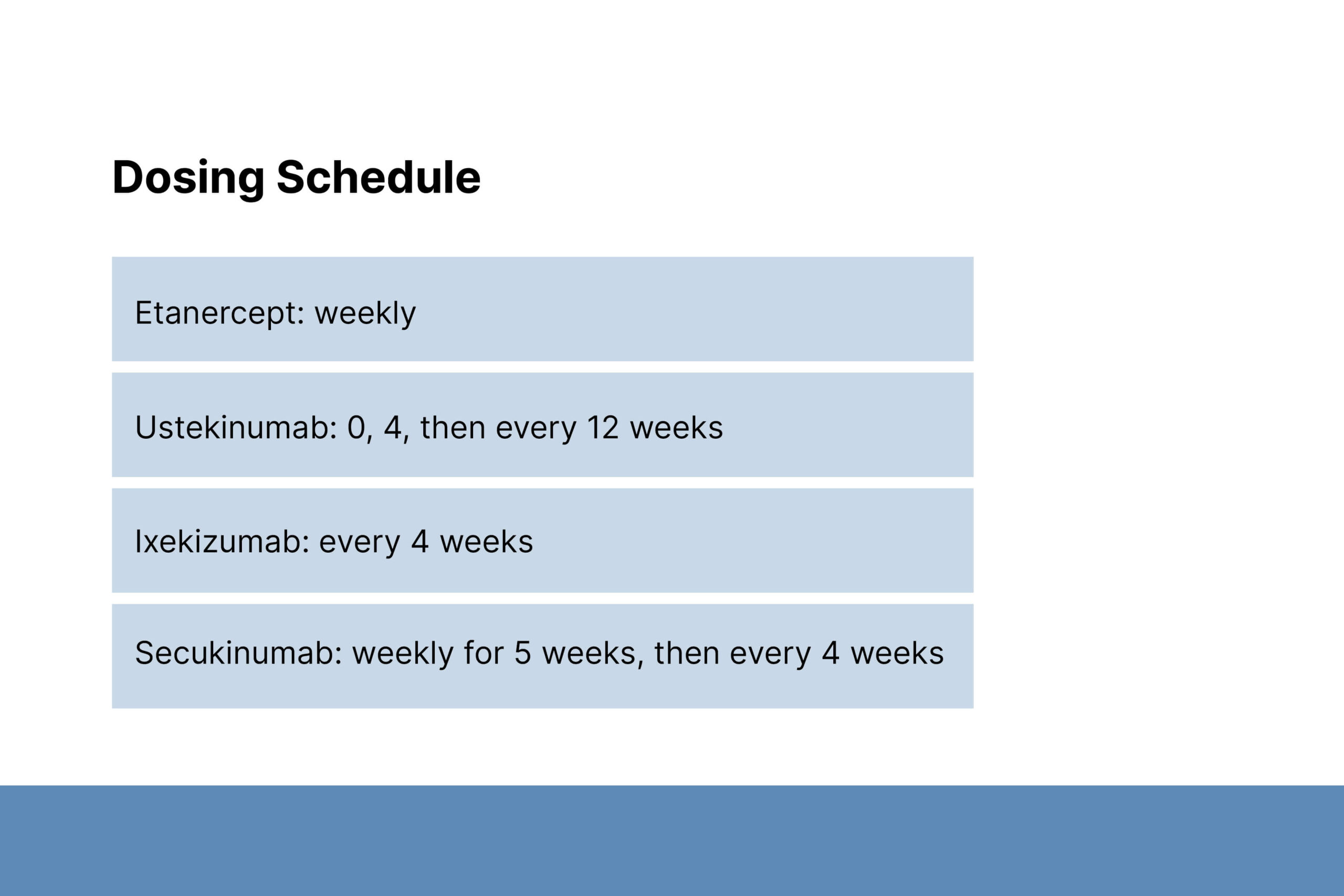
Third, Dr. Craiglow discussed FDA-approved biologics for pediatric psoriasis including etanercept, ustekinumab, ixekizumab, and secukinumab. She shared guidance for how to choose which medication is most appropriate for a given patient.
Finally, Dr. Craiglow emphasized that it is the dermatologist’s role to help pediatric patients learn to answer questions about their disease. She shared the formula from the organization Changing Faces: explain, reassure, redirect. For example, “I have eczema. I’m not sick, it’s not contagious, I just get rashes sometimes. Race you to the slide!”