Atopic Dermatitis: Guidelines of Care
David E. Cohen, MD, MPH
Charles C. and Dorothea E. Harris Professor and Executive Vice Chairman for Operations and Strategy,
The Ronald O. Perelman Department of Dermatology,
New York University Grossman School of Medicine
June 2024
Dr. Cohen presented information about the updated guidelines from the American Academy of Dermatology (AAD) for topical, systemic, and phototherapy treatments for atopic dermatitis (AD).
First, Dr. Cohen discussed updated AAD guidelines for topical therapies. Moisturizers, calcineurin inhibitors, topical corticosteroids, topical phosphodiesterase-4 (PDE-4) inhibitors, and Janus kinase (JAK) inhibitors are strongly recommended. Dr. Cohen encouraged clinicians to consider the amount of topical medication required to treat widespread disease. If AD extends beyond 8−10% of body surface area, he suggested considering phototherapy or systemic therapies.
Second, Dr. Cohen discussed updated guidelines for phototherapy and systemic therapies. The guidelines recommend these therapies in patients who are refractory to topical therapies. Dr. Cohen noted that the guidelines do not mention the severity of AD, giving clinicians freedom to choose when to use these treatments. Dr. Cohen recommended asking patients about comorbidities before starting systemic therapies because some may be indicated for multiple conditions.
Additional updated recommendations include:
- Conditional recommendation for phototherapy due to lack of evidence. There was insufficient data to recommend psoralen ultra-violet A (PUVA).
- Baricitinib was recommended due to robust data and European Medical Association approval. It is not FDA approved.
- Conditional recommendation against systemic corticosteroids. Dr. Cohen recognized that dermatologists often prescribe corticosteroids for flares or special events. This recommendation emphasizes that they should be considered a bridge treatment and not for long-term use.
- JAK inhibitors can be used in healthy adults but require laboratory monitoring. Caution is advised for people with increased risks of serious adverse events, including patients age ≥65 years, smokers, and those with increased risk of heart attack, stroke, cancer, or blood clots.
Third, Dr. Cohen described how he justifies systemic therapy use in clinical notes. The notes are brief but provide a clear picture of disease control. They include:
- Family and personal history of comorbidities such as asthma, eczema, and food allergies
- Numerical Rating Scale (NRS) for itch in the current moment and the worst itch in the last 24 hours
- Plaque locations
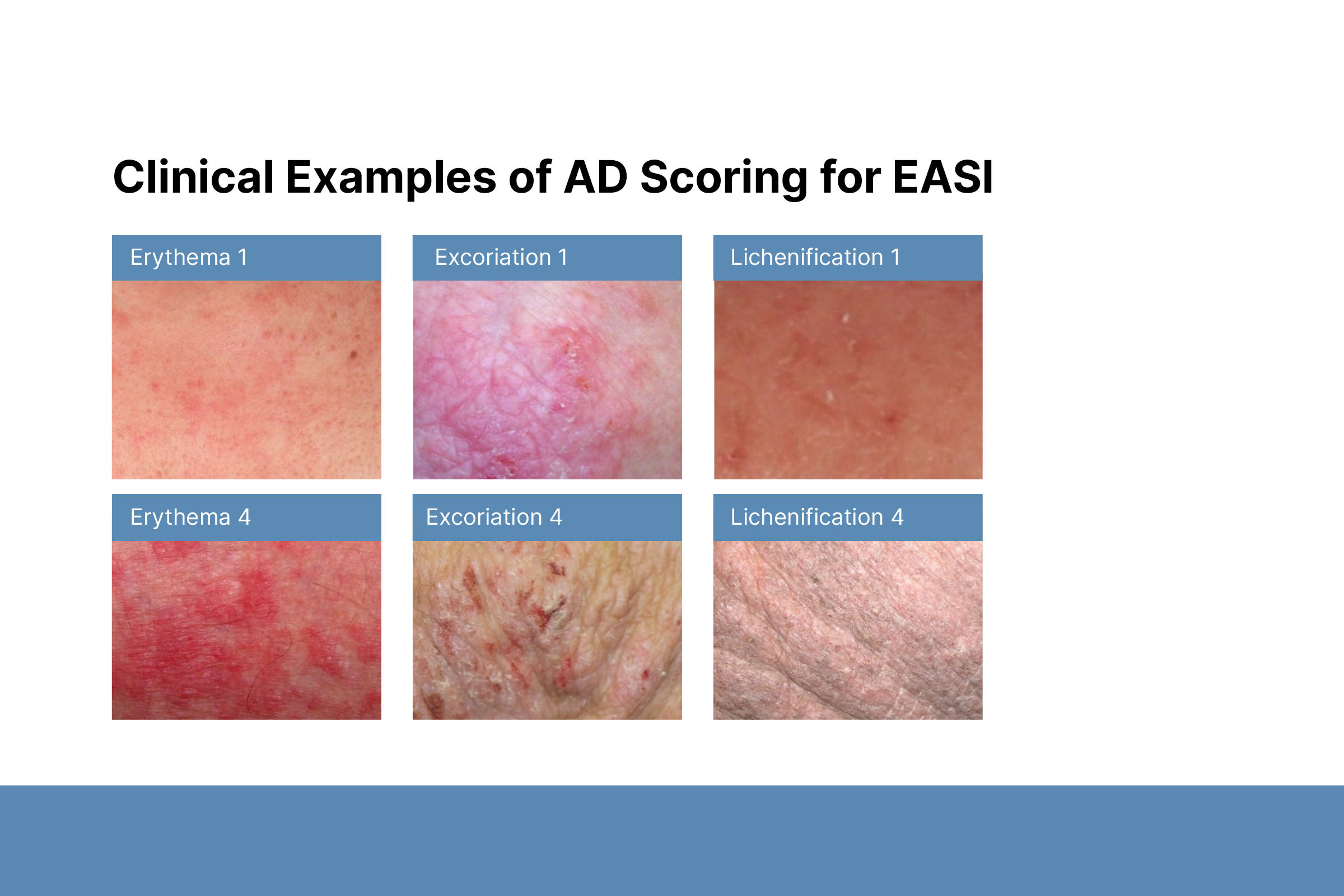
- Severity of erythema, scale/crust, and lichenification on a scale from 0 to 4
- Global assessment score 0–4
- Treatment start date
To conclude, Dr. Cohen emphasized that systemic therapies should be used in patients with moderate-to-severe AD who are refractory to topical treatment. Topical therapies should be used in conjunction with systemic therapies for maintenance of response, rescue, or treatment of flares.