A Country Doctor by Any Other Name
Robert T. Brodell, MD, 2024 DF Practitioner of the Year
June 2024

Dr. Robert Brodell, DF 2024 Practitioner of the Year, prides himself on being “just a country doctor.” Providing access to care in rural America has been the cornerstone of his career.
Devoted to patient care, academics, his family, and volunteerism since he received his medical degree from the University of Rochester School of Medicine and Dentistry in 1979, Dr. Brodell’s 40+-year career has included extensive clinical and teaching experience. Today he’s a dermatologist in Jackson, Mississippi, where he serves as Chairman of the Department of Pathology, Past Founding Chair of the Department of Dermatology and despite his administrative and dermatopathology duties, he still sees patients in the clinic four half days per week.
DF Practitioner of the Year Award: What it Takes
The DF Practitioner of the Year Award honors an individual who skillfully blends all professional activities with an enduring commitment to being a dermatologist and who provides the best possible clinical service to each patient. Each year, a colleague whose outstanding record of private practice and professional leadership establishes them as model physicians and examples of excellence and commitment for their colleagues and future generations of dermatologists is the recipient of this award.
Patient care in rural America
Dr. Brodell became a dermatologist by accident. During his internship in internal medicine at Strong Memorial Hospital in Rochester, New York, he planned to take over his father’s internal medicine practice in Warren, a city of less than 40,000 in northeastern Ohio where he grew up. His wife, Linda, who was two years behind him in medical school, wanted to be a general surgeon. They realized that both of these specialties require a lot of nights and potential urgent care that could impact their plans for a family. Coincidentally that week, his advisor introduced him to the Chief of Dermatology at Barnes Hospital/Washington University in St. Louis, Arthur Z. Eisen, MD, who had an open residency slot and asked Dr. Brodell if he wanted to be a dermatologist.
“As a proud internist, I remember thinking, ‘Hell no! It’s the internist who does the inspection component of the physical examination.’ But, I went to meet him, we hit it off, and the next thing I knew I was a dermatologist.” His wife, Linda P. Brodell, MD, chose ophthalmology.

Dr. Linda Brodell (right), and Dr. Robert Brodell’s mentor Dr. David Bickers (center) attended the awards ceremony.
In his final year of residency, Dr. Brodell was planning to work in a private practice for one year in St. Louis before returning home to Warren when another twist led him to dermatopathology.
“My father told me, ‘You’re never going to have an opportunity like this for the rest of your life. You’re at a first-rate university. Learn something more before you come home.’”
Taking the advice, he applied for a fellowship and spent a year as the first dermatopathology fellow of his mentor, Dr. Daniel Santa Cruz, who at the time was an Associate Professor at Barnes-Jewish Hospital and Washington University.
I want people to know they can be successful delivering care in solo practices in rural America.
He and Linda moved to Warren in 1985, where Dr. Brodell ran an independent certified dermatopathology laboratory and a dermatology office for 27 years. They lived in the same building which housed the dermatology and ophthalmology practices and skin pathology lab. They ran their practices like a family and, in fact, had five family members among their staff of 44 employees. Perhaps it is not a surprise that two of their five children, Lindsey Brodell Dolohanty, MD, and David William Brodell, MD, are dermatologists.
Dr. Brodell is passionate about dermatologic access to care. “We were able to do the kind of “small town” medicine that people did years ago,” he said.
The call of academia
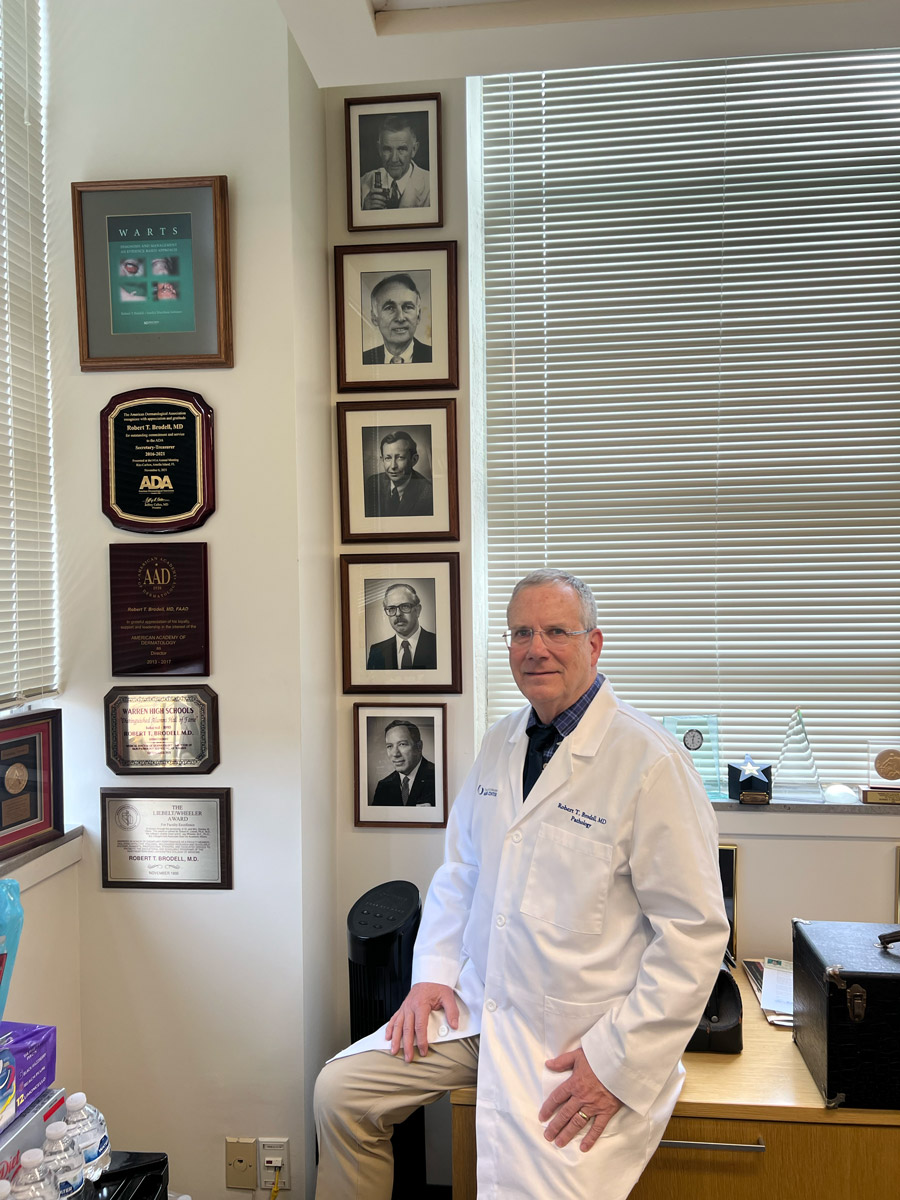
Photos of Dr. Brodell’s mentors line one of his office walls.
Dr. Brodell continued to explore academic medicine under the tutelage of his mentor, David R. Bickers, MD, who was the Chair of Dermatology at Case Western Reserve at the time.
“David Bickers helped me at every step. When he asked me what I was passionate about, I complained that the American Board of Dermatology (ABD) examination was not as clinically relevant as it should be. That’s when he told me he was president of the ABD,” Dr. Brodell laughed. “He asked me to write the kind of questions for the Board that I thought would be better.”
The ABD was rolling out maintenance of certifications and they also wanted him to explain the value of a system of recertification to private practitioners. With his experience in a dermatopathology lab and from his clinical practice, he wrote questions that focused on clinical-pathologic correlation that were well-received. After a couple of years on the question-writing committee, Dr. Brodell was elected to the Board, eventually becoming the President of the ABD (2011–2012).
A natural teacher
Dr. Brodell was an aggressive volunteer at Northeast Ohio Medical University (NEOMED), in Rootstown, Ohio while he continued to run his private practice. He soon rose to the rank of professor, won a series of teaching awards, and became Chief of the Dermatology section in the Department of Internal Medicine at NEOMED.
“Teaching medical students was fertile ground for me to experiment with a variety of teaching skills,” he said. “As well, getting to teach medical students at the bedside in a clinic gave me confidence that I could be an academic in the setting of a private practice.” Others agreed.
Dr. Brodell underscores the transformative effect of the Foundation’s early funding on investigators’ research.
In 2012, Dr. Brodell moved to Jackson, Mississippi as the founding Chair of the Department of Dermatology, partly on the strength of a teaching portfolio—that included more than 1,600 lectures and several hundred publications written by his students and residents. He had also developed leadership abilities at the American Cancer Society where he was a volunteer and rose through the ranks to the national Board. Dr. Brodell is in the ACS Relay for Life Hall of Fame, in part because he led a relay that raised over 7 million dollars for the society in his small town.
In Jackson, Dr Brodell recruited a team of dermatologists to develop dermatology offices and initiate a residency training program that has since grown to 15 faculty, representing all the dermatology subspecialties, and sees 65,000 patient visits a year. The faculty he recruited and residents who graduated and stayed in Mississippi now account for over 40% of the dermatologists in the state. The Department is nationally known for a model rural satellite office and rural dermatology residency training slot that is ensuring access to skin care to citizens of the state. In 2022, Dr. Brodell shifted over to become Chair of Pathology at the University.

Devotion to teaching, students and academia
All dermatologists have had cases that instill a passion for our work. One Tuesday “Dr Bob” was playing basketball in the clinic’s parking lot when a friend asked him to look at a compound nevus on his medial thigh. The man told him it had grown larger in the past six months and had become irritated. In the clinic, Dr. Brodell noted that the lesion looked like an irritated nevus, but biopsied the lesion immediately because it was changing. The lesion turned out to be a malignant melanoma, which was then surgically excised. Two years later the man died of widespread malignant melanoma. “It occurred to me that if I had not biopsied the lesion immediately, my friend’s death could have been attributed to any delay.
This entangled me in what has been called the “magnificent obsession”… the desire to diagnose melanoma at the earliest possible time.” This case study that led Dr. Brodell to recommend the expansion of the existing ABCD mnemonic for melanoma identification to include an E for enlargement or change (Hazen et al. 1999). This article is exemplary of the publications he co-wrote with students at NEOMED to support their career aspirations of being accepted to a dermatology program. He has published 450 articles, many co-authored by his students and residents, and has written three books. He is also the founding editor-in-chief of Practice Update: Dermatology and Associate Editor of the Journal of the American Academy of Dermatology.
It is possible
“When I went into solo private practice, 80 percent of dermatologists coming out of residency were doing the same,” Dr. Brodell said. “Now, that’s only one percent. The cost of running a practice is much higher and inflation-adjusted payments for physicians are down. You need a big enterprise to fill out all the forms and prior authorizations, as well as a hundred-thousand-dollar computer for medical records. Now graduates of dermatology residency training programs are working in group settings or in academic medicine instead.
“This kind of life isn’t easy, and you have to be prepared to fail at times, but I want people to know they can be successful delivering care in solo practices in rural America. Don’t let people tell you it can’t be done. Somebody early in my career told me, I could either do academics or private practice, but not both. That put a little burr up my behind to motivate me—and I’ve dedicated myself to proving the naysayers wrong.”
DF influence on specialty
“It was David Bickers who suggested I get involved with the Dermatology Foundation,” Dr. Brodell said. “While I wasn’t doing bench research of my own, I felt it was important to contribute to the Foundation’s support of young investigators who were developing the future tools to advance our field.” He became a member of the DF Annenberg Circle.
Dr. Brodell underscores the transformative effect of the Foundation’s early funding on investigators’ research. This initial support paved the way for investigators to reach their first research milestones, secure RO1 grants, and attract larger funding sources. “That’s what helped investigators generate knowledge that affects what clinicians do every day. I would say that’s a significant impact.”
That impact extends to networking. Dr. Brodell believes Foundation funding is as much about building networks as it is about financial support. “The Foundation’s annual Clinical Symposium is a meeting with significant opportunities for young investigators to learn and form collaborative relationships,” he said. “It’s a clinically oriented conference with excellent teachers selected for their ability to impart knowledge focusing on issues that impact private practice.”
Values to live and work by
During his private practice career, Dr. Brodell volunteered his time teaching residents at NEOMED, his alma mater University of Rochester, and at Case Western Reserve devoting about a half a day a month to teaching during his 27 years in Warren. He noted that these efforts enriched his life and cemented lasting relationships.
His combination of practice surrounded by family, devotion to his wife and kids, community outreach, teaching, public service in dermatology organizations, and philanthropy are a good example of what can be done when one sets one’s mind to a goal—or, in Dr. Brodell’s case, a series of goals.
“I’ve allowed myself to become passionate about things….and, always tried to reach a little higher,” he said. “I still feel that I’m living the dream.”
References
Hazen BP, Bhatia AC, Zaim T, Brodell RT. The clinical diagnosis of early malignant melanoma: expansion of the ABCD criteria to improve diagnostic sensitivity. Dermatol Online J. 1999;5(2):3. PMID: 10673456.
Brodell RT. Enlarging common melanocytic nevi and the diagnosis of malignant melanoma. Arch Dermatol. 2001;137:227.
Zaharna M. Brodell RT, It’s time for a “change” in our approach to early detection of malignant melanoma. Clin Dermatol. 2003; 21(5): 456-458.

