Acral and Nail Unit Melanoma: Challenges and Approaches to Diagnosis and Management
July 2025
Dr. Daniel Klufas presented information about the clinical presentation, diagnosis, and management of acral melanoma, including acral lentiginous melanoma (ALM) and nail unit melanoma (NUM). Acral melanomas are rare subtypes of cutaneous melanoma (CM) found on non-hair-bearing acral surfaces. They typically present after the age of 50 and disproportionately affect patients with skin of color and lower socio-economic status.
First, Klufas described the clinical presentation and diagnosis of acral melanomas. ALM is a distinct histopathologic subtype of melanoma that typically presents as an asymmetric pigmented lesion on the palm of the hand or sole of the foot. ALMs generally do not arise from pre-existing nevi and have distinct mutational patterns from other CMs. Suspicious lesions have an irregular pigment pattern, occur after the sixth decade of life, and have changed in appearance according to patient reports. Dermoscopy can help differentiate between benign and malignant lesions. Klufas recommends a punch or deep shave biopsy to capture the entire depth of the lesion and prevent under-staging.
NUM arises on the subungual, ungual, and periungual skin surfaces, usually the thumb or big toe. Two-thirds of NUM present as longitudinal melanonychia (LM). The differential diagnosis for LM includes melanocyte activation and non-melanocytic tumors. Other concerning features for NUM include heterogeneity in color, triangular band, dotted or dashed pigment pattern, and Hutchinson sign. Of note, up to 25% of NUMs are amelanotic. To diagnose NUM, Klufas recommends nail plate removal with nail matrix shave biopsy because this is the only way to fully visualize the nail matrix, where most NUM originate.
ALM and NUM have similar prognostic factors as other CMs but higher rates of recurrence and worse outcomes. Poorer prognosis is attributed to advanced stage at diagnosis, genetic variation, and socioeconomic disparities.
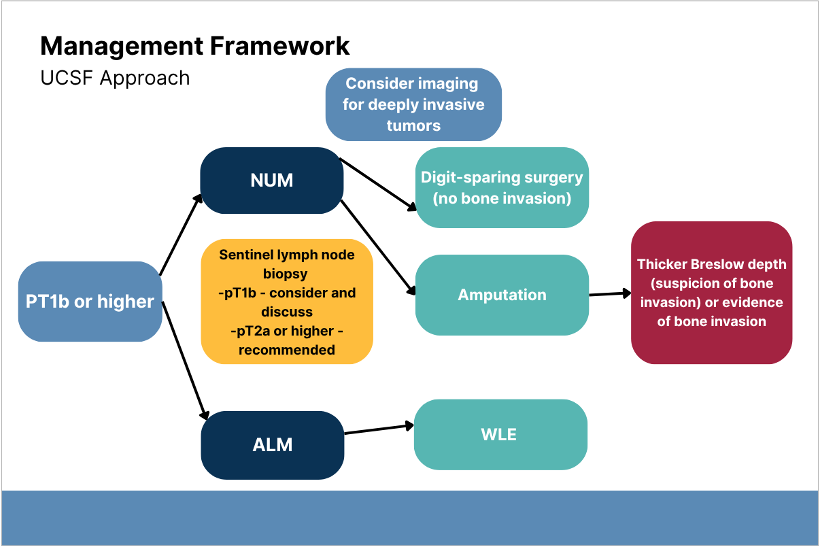
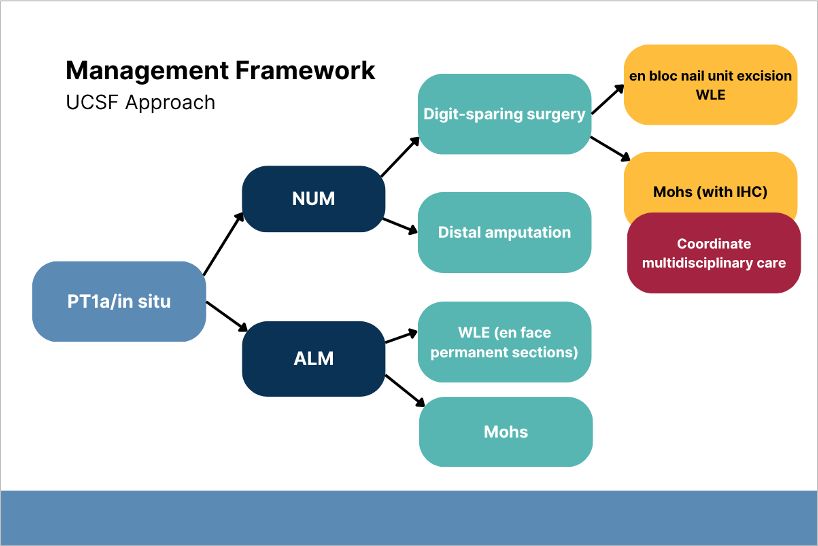
Third, Klufas described acral melanoma treatment and management. There are limited data and lack of consensus for acral melanoma surgical management. Klufas shared his management framework based on National Comprehensive Cancer Network guidelines. For ALM, he recommends wide local excision or Mohs surgery depending on tumor histopathology and patient preference. NUM surgical options differ based on melanoma thickness. Distal amputation should be considered for NUMs with thickness >0.8 mm or bony invasion.
If the tumor is less than 0.8 mm, presents no ulceration, and involves the nail unit, Dr. Klufas will recommend digit-sparing surgery but also discuss distal digit amputation.
When the tumor is greater than 0.8 mm and involves the nail, Dr. Klufas generally favors amputation, particularly as the Breslow depth gets thicker and if there is bone involvement.
Digit-sparing surgery (bloc nail unit excision or Mohs) is appropriate for NUMs with thickness ≤0.8 mm. Klufas recommends sentinel lymph node biopsy in patients at stage T2a or higher and encourages discussion for the need in patients with T1b tumors.
Patients with metastatic disease are referred to medical oncology for immunotherapy and possibly surgical oncology for resection. Metastatic ALMs or NUMs have worse prognosis compared to other CMs due to lower response rates to immune checkpoint inhibitors and lower mutational burden. Combination anti PD-L1 and CTLA4 treatment remains the best option despite being less effective compared with other CMs.
To conclude, Klufas reviewed unmet needs in acral melanoma care. Ongoing education for dermatologists and primary care providers about at-risk patient populations will improve early diagnosis. Consensus guidelines on the surgical management of acral melanoma are needed.
Mark January 28-31, 2026 on your calendar for the 2026 Annual DF Clinical Symposium.

